Scoliosis
| Scoliosis | |
|---|---|
| Classification and external resources | |
Scoliosis of Caucasian girl age 16; frontal X-ray, standing, clothed |
|
| ICD-10 | M41. |
Scoliosis (from Greek: skoliōsis meaning from skolios, "crooked")[1] is a medical condition in which a person's spine is curved from side to side. Although it is a complex three-dimensional deformity, on an x-ray, viewed from the rear, the spine of an individual with a typical scoliosis may look more like an "S" or a "C" than a straight line. It is typically classified as either congenital (caused by vertebral anomalies present at birth), idiopathic (cause unknown, sub-classified as infantile, juvenile, adolescent, or adult according to when onset occurred) or neuromuscular (having developed as a secondary symptom of another condition, such as spina bifida, cerebral palsy, spinal muscular atrophy or physical trauma). This condition affects approximately 20 million people in the United States.[2]
Contents |
Signs and symptoms
Patients who have reached skeletal maturity are less likely to have a worsening case. Some severe cases of scoliosis can lead to diminishing lung capacity, putting pressure on the heart, and restricting physical activities.
The signs of scoliosis can include:
- Uneven musculature on one side of the spine
- A rib prominence and/or a prominent shoulder blade, caused by rotation of the ribcage in thoracic scoliosis
- Uneven hips / leg lengths
- Slow nerve action (in some cases)
Associated conditions
Scoliosis is sometimes associated with other conditions such as Ehler-Danlos syndrome (hyperflexibility, 'floppy baby' syndrome, and other variants of the condition), Charcot-Marie-Tooth, Prader-Willi syndrome, kyphosis, cerebral palsy, spinal muscular atrophy, muscular dystrophy, familial dysautonomia, CHARGE syndrome, Friedreich's ataxia, proteus syndrome, spina bifida, Marfan's syndrome, neurofibromatosis, connective tissue disorders, congenital diaphragmatic hernia, and craniospinal axis disorders (e.g., syringomyelia, mitral valve prolapse, Arnold-Chiari malformation).
Cause
In the case of the most common form of scoliosis, adolescent idiopathic scoliosis, there is no clear causal agent and it is generally believed to be multifactorial. Genetics are believed to play a role.[3] Various causes have been implicated, but none has consensus among scientists as the cause of scoliosis, though the role of genetic factors in the development of this condition is widely accepted.[4]
Scoliosis is more often diagnosed in females. In some cases, scoliosis exists at birth due to a congenital vertebral anomaly. Occasionally, development of scoliosis during adolescence is due to an underlying anomaly such as a tethered spinal cord, but most often the cause is unknown or idiopathic, having been inherited through multiple factors, including genetics.[5] Scoliosis often presents itself, or worsens, during the adolescence growth spurt.
In April 2007, researchers at Texas Scottish Rite Hospital for Children[6] identified the first gene associated with idiopathic scoliosis, CHD7. The medical breakthrough was the result of a 10-year study and is outlined in the May 2007 issue of the American Journal of Human Genetics.[4]
Diagnosis
Patients who initially present with scoliosis are examined to determine whether there is an underlying cause of the deformity. During a physical examination, the following is assessed:
- Skin for café au lait spots indicative of neurofibromatosis
- The feet for cavovarus deformity
- Abdominal reflexes
- Muscle tone for spasticity
During the exam, the patient is asked to remove his or her shirt and bend forward. (This is known as the Adams Forward Bend Test[7] and is often performed on school students.) If a prominence is noted, then scoliosis is a possibility and the patient should be sent for an X-ray to confirm the diagnosis. Alternatively, a scoliometer may be used to diagnose the condition.[8] The patient's gait is assessed, and there is an exam for signs of other abnormalities (e.g., spina bifida as evidenced by a dimple, hairy patch, lipoma, or hemangioma). A thorough neurological examination is also performed.
It is usual, when scoliosis is suspected, to arrange for weight-bearing full-spine AP/coronal (front-back view) and lateral/sagittal (side view) X-rays to be taken, to assess the scoliosis curves and the kyphosis and lordosis, as these can also be affected in individuals with scoliosis. Full-length standing spine X-rays are the standard method for evaluating the severity and progression of the scoliosis, and whether it is congenital or idiopathic in nature. In growing individuals, serial radiographs are obtained at 3-12 month intervals to follow curve progression. In some instances, MRI investigation is warranted to look at the spinal cord.
The standard method for assessing the curvature quantitatively is measurement of the Cobb angle. The Cobb angle is the angle between two lines, drawn perpendicular to the upper endplate of the uppermost vertebrae involved and the lower endplate of the lowest vertebrae involved. For patients who have two curves, Cobb angles are followed for both curves. In some patients, lateral bending X-rays are obtained to assess the flexibility of the curves or the primary and compensatory curves.
Genetic testing
Genetic testing for AIS, which has become available in 2009 and is still under investigation, attempts to gauge the likelihood of curve progression.
Through a genome-wide association study, geneticists have identified single nucleotide polymorphism markers in the DNA that are significantly associated with adolescent idiopathic scoliosis. Fifty-three genetic markers have been identified. Scoliosis has been described as a biomechanical deformity, the progression of which is dependent on asymmetric forces otherwise known as the Heuter-Volkmann law.[9][10]
Management
The traditional medical management of scoliosis is complex and is determined by the severity of the curvature and skeletal maturity, which together help predict the likelihood of progression.
The conventional options are, in order:
- Observation
- Physical therapy
- Occupational Therapy
- Bracing
- Surgery
A growing body of scientific research testifies to the efficacy of specialized treatment programs of physical therapy, which may include bracing.[11] Debate in the scientific community about whether chiropractic and physical therapy can influence scoliotic curvature is partly complicated by the variety of methods proposed and employed: Some are supported by more research than others.[12]
Physiotherapy
The Schroth method is a noninvasive, physiotherapeutic treatment for scoliosis which has been used successfully in Europe since the 1920s.[13][14] Originally developed in Germany by scoliosis sufferer Katharina Schroth, this method is now taught to scoliosis patients in clinics specifically devoted to Schroth therapy in Germany, Spain, England and North America. The method is based upon the concept of scoliosis as resulting from a complex of muscular asymmetries (especially strength imbalances in the back) that can be at least partially corrected by targeted exercises.[14]
The Schroth method has proven effective at reversing abnormal scoliotic curvatures by an average of 10% in 4- to 6-week in-patient programs,[15] and by 30% or more in an out-patient program over a period of a year.[16] One study of nearly 200 adolescent Schroth patients found no curve progression three years following the in-patient program.[17] Several studies have documented the Schroth method's efficacy in substantially reducing or eliminating pain, which tends to be a problem particularly for adults.[18]
Small curvatures between 15 and 20° during growth may be treated with the physio-logic-program,[19] curvatures between 20 and 30° during growth spurt with "3D-made-easy". This program has been tested in the environment of inpatient treatment as well,[20][21] in curvatures exceeding 30° a combination of the methods described together with the Schroth program may be helpful.[22] A specialized centre with trained and certified staff should be taken into account. Out-patient rehabilitation treatments today may reach the same outcome as in-patient programs.[23] Out-patient programs may be successful when pattern-specific programs are provided. A certain intensity is necessary to allow the very best compliance with conservative treatment and to acquire strategies for coping with scoliosis and with the conservative treatment.
The indications for treatment depend on degree of curvature, maturity of the patient, and the individual curve pattern. While evidence supporting such conservative, non-invasive treatments is weak, today conservative management of scoliosis can be regarded as being evidence-based; no substantial evidence has been found to support surgical intervention.[24]
Occupational therapy
An occupational therapist (OT) helps those who have experienced an injury or illness regain or maintain the ability to participate in their everyday activities. For a person with scoliosis, an occupational therapist can provide assistance through assessment, intervention, and ongoing evaluation of the condition. This will help the person manage physical symptoms so they can participate in daily activities, notably in self-care, productivity and leisure.
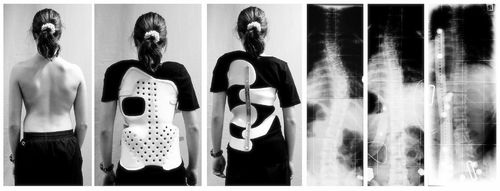
One intervention involves bracing. During the past several decades, a large variety of bracing devices have been developed for the treatment of scoliosis.[25] Studies demonstrate that presenting force sideways across a joint by bracing prevents further curvature of the spine in idiopathic scoliosis.[26] Other studies have also shown that braces can be used by individuals with scoliosis during physical activities.[27]
Other interventions include postural strategies such as posture training in sitting, standing and sleeping positions and using positioning supports such as pillows, wedges, rolls, and corsets.[28]
Adaptive and compensatory strategies are also employed to help facilitate individuals to returning daily activities.
Self-care
Disability caused by scoliosis, as well as physical limitations during recovery from treatment related surgery, often affect an individual’s ability to perform self-care activities.[29] One of the first treatments of scoliosis is the attempt to prevent further curvature of the spine. Depending on the size of the curvature, this is typically done in one of three ways: bracing, surgery, or postural positioning through customized cushioning.[29][30][31] Stopping the progression of the scoliosis can prevent the loss of function in many activities of daily living by maintaining range of motion, preventing deformity of the rib cage and reducing pain during activities such as bending or lifting.
Occupational therapists are often involved in the process of selection and fabrication of customized cushions. These individualized postural supports are used to maintain the current spinal curvature, or they can be adjusted to assist in the correction of the curvature. This type of treatment can help to maintain mobility for a wheelchair user by preventing the deformity of the rib cage and maintaining active range of motion in the arms.[29]
For other self-care activities (such as dressing, bathing, grooming, personal hygiene and feeding), several strategies can be used as a part of occupational therapy treatment. Environmental adaptations for bathing could include a bath bench, grab bars installed in the shower area, or a handheld shower nozzle.[32] For activities such as dressing and grooming, various assistive devices and strategies can be used to promote independence. An occupational therapist may recommend a long-handled reacher that can be used to assist independent dressing by allowing a person to avoid painful movements such as bending over; a long-handled shoehorn can be used for putting on and removing shoes. Problems with activities such as cutting meat and eating can be addressed by using specialized cutlery, kitchen utensils, or dishes.
Productivity
Productive activities include paid or unpaid work, household chores, school, work, and play.[33] Recent studies in health care have led to the development of a variety of treatments to assist in the management of scoliosis thereby maximizing productivity for people of all ages. Assistive technology has undergone dramatic changes over the past 20 years; the availability and quality of the technology has improved greatly.[34] As a result of using assistive technology, functional changes may range from improvements in abilities, performance in daily activities, participation levels, and quality of life.[33]
A common assistive technology intervention is specialized seating and postural control. It is widely known that, for children with poor postural control, a comfortable seating system that provides them with the support needed to maintain a sitting position can be essential for raising their overall level of well being.[35] A child's well-being in a productive sense involves the ability to participate in classroom and play activities.[33] Specialized wheelchair seating has been identified as the most common prescription in the management of scoliosis in teenagers with muscular dystrophy.[36]
With comfortable wheelchair seating, teenagers are able to participate in classroom activities for longer periods with less fatigue. By tilting the seating position 20 degrees forward (toward the thighs), seating pressure is significantly redistributed and, therefore, sitting is more comfortable. If an office worker with scoliosis can sit for longer periods, increased work output is likely to occur and could improve quality of life.
For those who do not use a wheelchair, bracing may be used to treat scoliosis. Lifestyle changes are made to compensate for the proper use of spine braces.
Leisure
Leisure activities include those activities that an individual finds meaningful and enjoyable. There are many physical symptoms that can prevent a person from engaging in physical leisurely activities, such as chest pains, back pains, shortness of breath, and limited spinal movement. The OT's role is to help individuals with scoliosis manage these physical symptoms so they can participate in physical leisure activities.
Bracing is a common strategy recommended by an OT, particularly for individuals engaging in sports and exercise.[27] An OT is responsible for educating an individual on the advantages and disadvantages of different braces, proper ways to wear the brace, and the day-to-day care of the brace.
To help a person manage heart and lung symptoms such as shortness of breath or chest pains, an occupational therapist can teach the individual energy conservation techniques.[32] This includes scheduling routine breaks during the activity, as suitable for the individual. For example, an occupational therapist can recommend that a swimmer take breaks between laps to conserve energy. Other energy conservation strategies knowing the benefits of scheduled rest and efficient breathing techniques.[32] Adapting or modifying the exercise or sport is another way a person with scoliosis can do it.[32] Adapting the activity may change the difficulty of the sport or exercise. For example, it might mean taking breaks throughout an exercise. If a person with scoliosis is unable to participate in a sport or exercise, an OT can help the individual explore other physical activities that are suitable to his/her interests and capabilities. An OT and the person with scoliosis can explore enjoyable and meaningful participation in the sport/exercise in another capacity, such as coaching or refereeing.
Bracing
Bracing is normally done when the patient has bone growth remaining and is generally implemented to hold the curve and prevent it from progressing to the point where surgery is recommended. Braces are sometimes prescribed for adults to relieve pain. Bracing involves fitting the patient with a device that covers the torso; in some cases it extends to the neck. The most commonly used brace is a TLSO, a corset-like appliance that fits from armpits to hips and is custom-made from fiberglass or plastic. It is usually worn 22–23 hours a day and applies pressure on the curves in the spine. The effectiveness of the brace depends not only on brace design and orthotist skill, but on patient compliance and amount of wear per day.
Typically, braces are used for idiopathic curves that are not grave enough to warrant surgery, but they may also be used to prevent the progression of more severe curves in young children, to buy the child time to grow before performing surgery, which would prevent further growth in the part of the spine affected.
Bracing may cause emotional and physical discomfort. Physical activity may become more difficult because the brace presses against the stomach, making it difficult to breathe. Children may lose weight from the brace, due to increased pressure on the abdominal area.
The Scoliosis Research Society's recommendations for bracing include curves progressing to larger than 25 degrees, curves presenting between 30 and 45 degrees, Risser Sign 0, 1, or 2 (an x-ray measurement of a pelvic growth area), and less than 6 months from the onset of menses in girls.[37]
Progressive scolioses exceeding 25° Cobb in the pubertal growth spurt should be treated with a pattern specific brace like the Chêneau brace and its derivates with an average brace wearing time of 16 hours/day (23 hours/day assures the best possible result).
The latest standard of brace construction is with CAD/CAM technology. With the help of this technology it has been possible to standardize the pattern specific brace treatment. Severe mistakes in brace construction are largely ruled out with the help of these systems. This technology also eliminates the need to make a plaster cast for brace construction. The measurements can be taken any place and is simple (and not comparable to plastering). In Germany available CAD/CAM braces are known such as the Regnier-Chêneau brace, the Rigo-System-Chêneau-brace (RSC brace), and the Gensingen Brace according to Weiss.[38] Many patients prefer the "Chêneau light" brace: It has the best in-brace corrections reported in international literature and is easier to wear than other braces in use today.[39][40] However, this brace is not available for all curve patterns.
A more recent development is the SpineCor Dynamic brace. It was developed by a research team at the St. Justine Hospital in Montreal Canada, as part of a research project funded by the Canadian government. The brace was first used in clinical application in Montreal in 1992 and is currently used in many countries throughout the world.
This brace works using a different treatment approach to rigid bracing. Rather than trying to force the spine straight using three points of pressure, SpineCor uses a corrective movement. The regions of the body — shoulders, rib cage, lumbar spine and pelvis — are guided to a postural position that is the inverse of the scoliotic posture. As the spine is connected to the body it must move with the body when it is repositioned by the corrective movement. Hence, through the coupling of postural and spinal position, it is possible to affect the geometry of the scoliotic curve.
The advantages of SpineCor are that is flexible and allows dynamic movement, thereby eliminating the muscle weakening side effects seen with rigid bracing. It is also very easily concealed under clothing. The fact that it works as both a rehabilitation device and a brace, means that corrections made in the brace are sustained over the long term in 95.7% of cases.
When correctly applied SpineCor Dynamic bracing has been shown to be one of the most a successful conservative treatments in the management of idiopathic scoliosis. The two largest bracing studies following the 2005 Scoliosis Research Society guidelines[41] were published in the Journal of Paediatric Orthopaedics in June 2007. One study conducted at the Rainbow Children’s Hospital[42] reported the effectiveness of TLSO and Providence bracing. The other conducted at the St. Justine Children’s Hospital[43] reported the effectiveness of the SpineCor brace. Both studies followed the Scoliosis Research Society guidelines, meaning they used the same inclusion and reporting criteria therefore making it possible to compare the results of the three groups.
These results found that SpineCor was 76.5% effective in avoiding surgery, Providence nighttime brace was 40% effective in avoiding surgery, and TSLO was 21% effective in avoiding surgery. Comparison of these results shows that SpineCor was 71% more effective in reducing the rate of surgery compared to TLSO.
Some authors have criticized the results of the SpineCor group,[44] claiming that these results have not been reproduced by centres independent of the inventors. However independent results have been published by centres in the UK,[45], Poland,[46][47] Spain,[48] and Greece.[49] Each of these studies show results comparable to those achieved at the St. Justine Hospital studies.
Two studies have shown negative results using SpineCor.[50][51] These studies have been heavily criticised for their poor methodology and conflicts of interest. In one study, the application of the SpineCor brace was used by the author in a way that the SpineCor was not designed for. The author also had no previous experience in fitting SpineCor and failed to declare a conflict of interest as the author had a vested commercial and intellectual interest in the brace to which SpineCor was being compared. In the second study SpineCor was applied by a group of partially trained practitioners who fitted the brace missing key components.[51] What these two studies show is that for SpineCor to be an effective treatment for idiopathic scoliosis, it must be applied by skilled practitioners who have completed the formal training program and fit the brace according to its intended use.
In infantile and sometimes juvenile scoliosis, a plaster jacket applied early may be used instead of a brace. It has been proven possible[52] to permanently correct cases of infantile idiopathic scoliosis by applying a series of plaster casts (EDF: elongation, derotation, flexion) on a specialized frame under corrective traction, which helps to "mould" the infant's soft bones and work with their growth spurts. This method was pioneered by UK scoliosis specialist Min Mehta. Today, however, CAD/CAM braces are available for young children with a certain standard. Therefore plaster jackets are now generally regarded as outdated.[38]
Surgery
 |
 |
|
|
Pre op (left) and post op (right) X-ray of a person with thoracic dextroscoliosis and lumbar levoscoliosis. The X-ray is projected such that the right side of the subject is on the right side of the image, i.e., the subject is viewed from the rear. This projection is typically used by surgeons as it is how surgeons see their patients when they are on the operating table. Surgery was a fusion and instrumentation.
|
||
Surgery is usually recommended by orthopedists for curves that have a high likelihood of progression (i.e., greater than 45 to 50 degrees magnitude), curves that would be cosmetically unacceptable as an adult, curves in patients with spina bifida and cerebral palsy that interfere with sitting and care, and curves that affect physiological functions such as breathing.
Surgery for scoliosis is performed by a surgeon who specializes in spine surgery. For various reasons it is usually impossible to completely straighten a scoliotic spine, but in most cases significant corrections are achieved.
While surgery may be deemed necessary in some cases, in many cases it is not. Paul Harrington, known for inventing the surgery that implants metal rods in scoliotic spines, stated in 1963, "metal does not cure the disease" of scoliosis, which is a condition involving much more than the spinal column.
There are two main types of surgery
- Anterior fusion: This surgical approach is through an incision (cut) at the side of the chest wall;
- Posterior fusion: This surgical approach is through an incision on the back and involves the use of metal instrumentation to correct the curve.
One or both of these surgical procedures may be needed. The surgery may be done in one or two stages and, on average, will take four to eight hours.
Spinal fusion with instrumentation
Spinal fusion is the most widely performed surgery for scoliosis. In this procedure, bone (either harvested from elsewhere in the body autograft or from a donor allograft) is grafted to the vertebrae so that when it heals they will form one solid bone mass and the vertebral column becomes rigid. This prevents worsening of the curve, at the expense of some spinal movement. This can be performed from the anterior (front) aspect of the spine by entering the thoracic or abdominal cavity or, more commonly, performed from the back (posterior). A combination is used in more severe cases.
Originally, spinal fusions were done without metal implants. A cast was applied after the surgery, usually under traction to pull the curve as straight as possible and then hold it there while fusion took place. Unfortunately, there was a relatively high risk of pseudarthrosis (fusion failure) at one or more levels and significant correction could not always be achieved.
In 1962, Paul Harrington introduced a metal spinal system of instrumentation that assisted with straightening the spine, as well as holding it rigid while fusion took place. The original (now obsolete) Harrington rod operated on a ratchet system, attached by hooks to the spine at the top and bottom of the curvature that when cranked would distract, or straighten, the curve. A major shortcoming of the Harrington method was that it failed to produce a posture where the skull would be in proper alignment with the pelvis and it didn't address rotational deformity. As a result, unfused parts of the spine would try to compensate for this in the effort to stand up straight. As the person aged, there would be increased wear and tear, early-onset arthritis, disc degeneration, muscular stiffness and pain with eventual reliance on painkillers, further surgery, inability to work full-time, and disability. "Flatback" became the medical name for a related complication, especially for those who had lumbar scoliosis.
Modern spinal systems are attempting to address sagittal imbalance and rotational defects unresolved by the Harrington rod system. They involve a combination of rods, screws, hooks and wires fixing the spine and can apply stronger, safer forces to the spine than the Harrington rod. This technique is known as the Cotrel-Dubousset instrumentation, currently the most common technique for the procedure.
Modern spinal fusions generally have good outcomes with high degrees of correction and low rates of failure and infection. Patients with fused spines and permanent implants tend to have normal lives with unrestricted activities when they are younger; it remains to be seen whether those that have been treated with the newer surgical techniques develop problems as they age.
Pedicle screw only posterior spinal fusion may improve major curve correction at 2 years among patients with adolescent idiopathic scoliosis (AIS) as compared to hybrid instrumentation (proximal hooks with distal pedicle screws) (65% versus 46%) according to a retrospective matched cohort study.[53] The prospective cohorts were matched to the retrospective cohorts according to patient age, fusion levels, Lenke curve type, and operative method. The two groups were not significantly different in regard to age, Lenke AIS curve type, or Riser grade. The numbers of fused vertebrae were significantly different (11.7±1.6 for pedicle screw versus 13.0±1.2 for hybrid group). This study's results may be biased due to the pedicle screw group being analyzed prospectively versus retrospective analysis of the hybrid instrumentation group.
In cases where scoliosis has caused a significant deformity resulting in a rib hump, it is often possible to perform a surgery called a costoplasty (also called a thorocoplasty) to achieve a better cosmetic result. This procedure may be performed at any time after a fusion surgery, whether as part of the same operation or several years after. It is usually impossible to completely straighten and untwist a scoliotic spine, and it should be noted that the level of cosmetic success will depend on the extent to which the fused spine still rotates out into the ribcage. A rib hump is evidence that there is some rotational deformity to the spine.
Complications
The risk of undergoing surgery for scoliosis is estimated to be 5%. Possible complications may be inflammation of the soft tissue or deep inflammatory processes, breathing impairments, bleeding and nerve injuries. However, according to the latest evidence, the rate of complications is far beyond that rate. As early as five years after surgery another 5% require reoperation and today it is not yet clear what to expect from spine surgery in the long-term.[54][55] Taking into account that signs and symptoms of spinal deformity cannot be changed by surgical intervention, surgery remains primarily a cosmetic indication, only especially in patients with adolescent idiopathic scoliosis (AIS), the most common form of scoliosis never exceeding 80°.[54][56] Unfortunately the cosmetic effects of surgery are not necessarily stable.[54]
In case one decides to undergo surgery a specialized center should be preferred.
Surgery without fusion
New implants have been developed that aim to delay spinal fusion and to allow more spinal growth in young children. For the youngest patients, whose thoracic insufficiency compromises their ability to breathe and applies significant cardiac pressure, ribcage implants that push the ribs apart on the concave side of the curve may be especially useful. These vertical expandable prosthetic titanium ribs (VEPTR) provide the benefit of expanding the thoracic cavity and straightening the spine in all three dimensions while allowing it to grow.
The other alternative in the growing child is a spine-to-spine growing rod system that avoids fusing the entire curve, but requires biannual surgery through limit incisions to lengthen the rods and spine. Although these methods are novel and promising, these treatments are only suitable for growing patients.
Prognosis
The prognosis of scoliosis depends on the likelihood of progression. The general rules of progression are that larger curves carry a higher risk of progression than smaller curves, and that thoracic and double primary curves carry a higher risk of progression than single lumbar or thoracolumbar curves. In addition, patients who have not yet reached skeletal maturity have a higher likelihood of progression (i.e., if the patient has not yet completed the adolescent growth spurt).
Epidemiology
A scoliosis spinal columns curve of 10° or less affects 1.5% to 3% of individuals.[37] The prevalence of curves less than 20° is about equal in males and females. It is most common during late childhood, particularly in girls.[57]
Society and culture
Scoliosis Research Society
The Scoliosis Research Society is a professional organization of physicians and allied health personnel. Their primary focus is on providing continuing medical education for health care professionals and on funding/supporting research in spinal deformities. Founded in 1966, the SRS has gained recognition as one of the world's premier spine societies. Strict membership criteria ensure that the individual Fellows support that commitment. Current membership includes over 1,000 of the world's leading spine surgeons as well as some researchers, physician assistants, and orthotists who are involved in research and treatment of spinal deformities. The purpose of the Scoliosis Research Society is to foster the optimal care of all patients with spinal deformities.[58]
About Skolyoz Destek Grubu
Skolyoz Destek Grubu is a non-profit network organization of Scoliosis patient groups, provides information on the diagnosis, treatment and care of persons living with scoliosis and supports its member organisations in the fulfilment of their missions.
Skolyoz Destek Grubu also advocates, both independently and in collaboration with organisations with similar objectives.
See also
- Kyphosis
- Hyperkyphosis
- Kyphoscoliosis
- Lordosis
- Pott's disease
- Scheuermann's disease
References
- ↑ Online Etymology Dictionary. Douglas Harper, Historian. Accessed 27 December 2008. Dictionary.com
- ↑ Good, Christopher (2009). "The Genetic Basis of Adolescent Idiopathic Scoliosis". Journal of the Spinal Research Foundation 4 (1): 13–5. http://www.spinemd.com/publications/articles/the-genetic-basis-of-adolescent-idiopathic-scoliosis.
- ↑ Kouwenhoven JW, Castelein RM (2008). "The pathogenesis of adolescent idiopathic scoliosis: review of the literature". Spine 33 (26): 2898–908. doi:10.1097/BRS.0b013e3181891751. PMID 19092622.
- ↑ 4.0 4.1 Ogilvie JW, Braun J, Argyle V, Nelson L, Meade M, Ward K (2006). "The search for idiopathic scoliosis genes". Spine 31 (6): 679–81. doi:10.1097/01.brs.0000202527.25356.90. PMID 16540873.
- ↑ "Scoliosis — Causes — Risk Factors". PediatricHealthChannel. http://www.pediatrichealthchannel.com/scoliosis/causes.shtml.
- ↑ Texas Scottish Rite Hospital for Children
- ↑ "Scoliosis symptoms — pain, flat back, screening, self-assessment". iscoliosis.com. http://www.iscoliosis.com/symptoms.html.
- ↑ "Scoliometer (Inclinometer)". National Scoliosis Foundation. http://www.scoliosis.org/store/scoliometer.php.
- ↑ US patent 6,773,437, Ogilvie J, Drewry TD, Sherman MC, Saurat J, "Shape memory alloy staple", issued 2004-08-10
- ↑ Ogilvie J (2010). "Adolescent idiopathic scoliosis and genetic testing". Current Opinion in Pediatrics 22 (1): 67–70. doi:10.1097/MOP.0b013e32833419ac. PMID 19949338.
- ↑ Negrini S, Fusco C, Minozzi S, Atanasio S, Zaina F, Romano M (2008). "Exercises reduce the progression rate of adolescent idiopathic scoliosis: results of a comprehensive systematic review of the literature". Disability and Rehabilitation 30 (10): 772–85. doi:10.1080/09638280801889568. PMID 18432435.
- ↑ Majdouline Y, Aubin CE, Robitaille M, Sarwark JF, Labelle H (2007). "Scoliosis correction objectives in adolescent idiopathic scoliosis". Journal of Pediatric Orthopedics 27 (7): 775–81. doi:10.1097/BPO.0b013e31815588d8 (inactive 2010-08-01). PMID 17878784.
- ↑ Lehnert-Schroth C (2000). Dreidimensionale Skoliosebehandlung (6th ed.). Stuttgart: Urban & Schwarzer.
- ↑ 14.0 14.1 Lehnert-Schroth C (2007). Three-Dimensional Treatment for Scoliosis: A Physiotherapeutic Method for Deformities of the Spine. Palo Alto CA: The Martindale Press. pp. 1–6. ISBN 0914959026.
- ↑ Weiss, HR (1992). "Influence of an in-patient exercise program on scoliotic curve.". Italian journal of orthopaedics and traumatology 18 (3): 395–406. PMID 1308886.
- ↑ Otman, S; Kose, N; Yakut, Y (2005). "The efficacy of Schroth s 3-dimensional exercise therapy in the treatment of adolescent idiopathic scoliosis in Turkey.". Saudi medical journal 26 (9): 1429–35. PMID 16155663.
- ↑ Weiss, HR; Lohschmidt, K; El-Obeidi, N; Verres, C (1997). "Preliminary results and worst-case analysis of in patient scoliosis rehabilitation.". Pediatric rehabilitation 1 (1): 35–40. PMID 9689236.
- ↑ Weiss HR, "Scoliosis-related pain in adults: Treatment influences," European Journal of Physical Medicine and Rehabilitation 3/3 (1993): 91-94.
- ↑ Weiss HR, Klein R (2006). "Improving excellence in scoliosis rehabilitation: a controlled study of matched pairs". Pediatric Rehabilitation 9 (3): 190–200. doi:10.1080/13638490500079583. PMID 17050397.
- ↑ Weiss HR, Hollaender M, Klein R (2006). "ADL based scoliosis rehabilitation--the key to an improvement of time-efficiency?". Studies in Health Technology and Informatics 123: 594–8. PMID 17108494. http://booksonline.iospress.nl/Extern/EnterMedLine.aspx?ISSN=0926-9630&Volume=123&SPage=594.
- ↑ Weiss HR, Maier-Hennes A (2008). "Specific exercises in the treatment of scoliosis--differential indication". Studies in Health Technology and Informatics 135: 173–90. PMID 18401090. http://booksonline.iospress.nl/Extern/EnterMedLine.aspx?ISSN=0926-9630&Volume=135&SPage=173.
- ↑ Weiss HR (2010). Best Practice in Conservative Scoliosis Care (3rd ed.). Munich: Pflaum.
- ↑ Rigo M, Quera-Salvá G, Villagrasa M, et al. (2008). "Scoliosis intensive out-patient rehabilitation based on Schroth method". Studies in Health Technology and Informatics 135: 208–27. PMID 18401092. http://booksonline.iospress.nl/Extern/EnterMedLine.aspx?ISSN=0926-9630&Volume=135&SPage=208.
- ↑ Weiss HR, Goodall D (2008). "The treatment of adolescent idiopathic scoliosis (AIS) according to present evidence. A systematic review". European Journal of Physical and Rehabilitation Medicine 44 (2): 177–93. PMID 18418338. http://www.minervamedica.it/index2.t?show=R33Y2008N02A0177.
- ↑ DeWald, RL (2003). Spinal Deformitities: The Comprehensive Text. New York: Thieme Medical Publishers, Inc.
- ↑ Bulthuis G.J., Veldhuizen A.G., Nijenbanning G. (2008). "Clinical effect of continuous corrective force delivery in the non-operative treatment of idiopathic scoliosis: a prospective cohort study of the TriaC-brace". European Spine Journal 17 (2): 231–239. doi:10.1007/s00586-007-0513-9. PMID 17926071.
- ↑ 27.0 27.1 Green BN, Johson C, Moreau C. (2009). "Is physical activity contraindicated for individuals with scoliosis? A systematic literature review". Journal of Chiropractic Medicine 8 (1): 25–37. doi:10.1016/j.jcm.2008.11.001. PMID 19646383.
- ↑ Paris MJ, Lang G, Benjamin MJ, Wilcox R. (2008). Standard of Care: Marfan Syndrome. Brigham and Womans Hospital. http://www.brighamandwomens.org/RehabilitationServices/Physical%20Therapy%20Standards%20of%20Care%20and%20Protocols/General%20-%20Marfan%20Syndrome.pdf.
- ↑ 29.0 29.1 29.2 Burd TA, Pawelek L, Lenke LG. (2008). "Upper Extremity Functional Assessment After Anterior Spinal Fusion via Thoracotomy for Adolescent Idiopathic Scoliosis: Prospective Study of Twenty-Five Patients". Spine 27 (1): 65–71. doi:10.1097/00007632-200201010-00016. PMID 11805638.
- ↑ Voda S. (2009). "Dangerous Curves: Treating adult idiopathic scoliosis". Nursing 39 (12): 42–46. doi:10.1097/01.NURSE.0000365025.40773.4c (inactive 2010-05-12). PMID 19934743.
- ↑ Weiss H.F. (2003). "Rehabilitation of adolescent patients with scoliosis – What do we know? A review of the literature". Pediatric Rehabilitation 6 (3): 183–194.
- ↑ 32.0 32.1 32.2 32.3 Radomski, M.V. (2008). Occupational therapy for physical dysfunction sixth edition.. Philadelphia: Lippincott Williams & Wilkins. p. 964. ISBN 978-0-7817-6312-7. http://books.google.com/?id=hczaxaAXCDsC&pg=PA964.
- ↑ 33.0 33.1 33.2 Rigby, P.J. (2009). Assistive technology for persons with physical disabilities: Evaluation and outcomes Thesis, Utrecht University, The Netherlands.. Toronto: University of Toronto Press. ISBN 978-90-393-50416.
- ↑ Salter K, Jutai J, Teasell R, Foley NC, Bitensky J, Bayley M. (2010). "Issues for selection of outcome measures in stroke rehabilitation: ICF activity". Disability and Rehabilitation 27 (6): 315–340. doi:10.1080/09638280400008545. PMID 16040533.
- ↑ Telfer S., Solomonidis S., Spence W. (2009). "An investigation of teaching staff members' and parents' views on the current state of adaptive seating technology and provision". Disability & Rehabilitation: Assistive Technology 5 (1): 14–24. doi:10.3109/17483100903191334. PMID 19941437.
- ↑ Richardson M & Frank A.O. (2009). "Electric powered wheelchairs for those with muscular dystrophy: problems of posture, pain and deformity". Disability & Rehabilitation: Assistive Technology 4 (3): 181–8. doi:10.1080/17483100802543114.
- ↑ 37.0 37.1 Herring JA (2002). Tachdjian's Pediatric Orthopaedics. Philadelphia PA: W.B. Saunders. ISBN 0721656846.
- ↑ 38.0 38.1 Weiss HR: Best Practice in conservative scoliosis care. Pflaum Company, 3rd. edition, Munich 2010
- ↑ Weiss HR, Werkmann M, Stephan C (2007). "Correction effects of the ScoliOlogiC "Chêneau light" brace in patients with scoliosis". Scoliosis 2: 2. doi:10.1186/1748-7161-2-2. PMID 17257399.
- ↑ Weiss HR, Werkmann M, Stephan C (2007). "Brace related stress in scoliosis patients - Comparison of different concepts of bracing". Scoliosis 2: 10. doi:10.1186/1748-7161-2-10. PMID 17708766.
- ↑ Richards, BS; Bernstein, RM; D'amato, CR; Thompson, GH (2005). "Standardization of criteria for adolescent idiopathic scoliosis brace studies: SRS Committee on Bracing and Nonoperative Management.". Spine 30 (18): 2068–75; discussion 2076–7. doi:10.1097/01.brs.0000178819.90239.d0. PMID 16166897. http://www.spinecor.co.kr/new/pdf/Richards%20et%20al%202005.pdf.
- ↑ Janicki, JA; Poe-Kochert, C; Armstrong, DG; Thompson, GH (2007). "A comparison of the thoracolumbosacral orthoses and providence orthosis in the treatment of adolescent idiopathic scoliosis: results using the new SRS inclusion and assessment criteria for bracing studies.". Journal of pediatric orthopedics 27 (4): 369–74. doi:10.1097/01.bpb.0000271331.71857.9a (inactive 2010-08-01). PMID 17513954.
- ↑ Coillard, C; Vachon, V; Circo, AB; Beauséjour, M; Rivard, CH (2007). "Effectiveness of the SpineCor brace based on the new standardized criteria proposed by the scoliosis research society for adolescent idiopathic scoliosis.". Journal of pediatric orthopedics 27 (4): 375–9. doi:10.1097/01.bpb.0000271330.64234.db (inactive 2010-08-01). PMID 17513955.
- ↑ Weiss, HR (2008). "SpineCor vs. natural history - explanation of the results obtained using a simple biomechanical model.". Studies in health technology and informatics 140: 133–6. PMID 18810014.
- ↑ K. Hassan (2006). "A Retrospective Analysis Of The SpineCor Brace Treatment At The Sheffield Children’s Hospital (S.C.H.), United Kingdom". Journal of Bone and Joint Surgery - British Volume 90-B (SUPP_III, 477): 477. http://proceedings.jbjs.org.uk/cgi/content/abstract/90-B/SUPP_III/477-c.
- ↑ Tomasz Potaczek et. al (2008). [http://www.rehmed.pl/images/upload/pdf_en/2008/2_2008/MEDICAL%20REHABILITATION%202-2008%20(1-6).pdf "The Early Results Of The Treatment Of Idiopathic Scoliosis Using The Dynamic SpineCor Brace"]. Medical Rehabilitation 12 (2): 1–6. http://www.rehmed.pl/images/upload/pdf_en/2008/2_2008/MEDICAL%20REHABILITATION%202-2008%20(1-6).pdf.
- ↑ Jacek Durmała et al. (2007). "Preliminary Results Of Use Of SpineCor Brace In Katowice (Poland)". Ann. Acad. Med. Siles 61: 1. http://early-onset-scoliosis.com/Documents/Preliminary%20results%20of%20use%20of%20SpineCor%20brace%20in%20Poland.pdf.
- ↑ Vera Miller A. (2009). Initial Results Of Spinecor Treatment Of Adolescent Idiopathic Scoliosis In Seville.
- ↑ Irini Tsakiri; Vakaloglou, Vangelis; Karvounis, Kostantinos; Kattou, Petros; Soucacos, Panagiotis K (2009). "The Use Of The SpineCor Dynamic Corrective Brace In Greece: A Preliminary Report". Scoliosis 4: O35. doi:10.1186/1748-7161-4-S1-O35. http://www.biomedcentral.com/content/pdf/1748-7161-4-S1-O35.pdf.
- ↑ Weiss, HR; Weiss, GM (2005). "Brace treatment during pubertal growth spurt in girls with idiopathic scoliosis (IS): a prospective trial comparing two different concepts.". Pediatric rehabilitation 8 (3): 199–206. doi:10.1080/13638490400022212. PMID 16087554.
- ↑ 51.0 51.1 Wong, MS; Cheng, JC; Lam, TP; Ng, BK; Sin, SW; Lee-Shum, SL; Chow, DH; Tam, SY (2008). "The effect of rigid versus flexible spinal orthosis on the clinical efficacy and acceptance of the patients with adolescent idiopathic scoliosis.". Spine 33 (12): 1360–5. doi:10.1097/BRS.0b013e31817329d9. PMID 18496349. http://early-onset-scoliosis.com/Documents/Wong%20Spinecor%20Study.pdf.
- ↑ Mehta MH (2005). "Growth as a corrective force in the early treatment of progressive infantile scoliosis". The Journal of Bone and Joint Surgery. British Volume 87 (9): 1237–47. doi:10.1302/0301-620X.87B9.16124. PMID 16129750.
- ↑ Kim YJ, Lenke LG, Kim J, et al. (2006). "Comparative analysis of pedicle screw versus hybrid instrumentation in posterior spinal fusion of adolescent idiopathic scoliosis". Spine 31 (3): 291–8. doi:10.1097/01.brs.0000197865.20803.d4. PMID 16449901.
- ↑ 54.0 54.1 54.2 Hawes M (2006). "Impact of spine surgery on signs and symptoms of spinal deformity". Pediatric Rehabilitation 9 (4): 318–39. PMID 17111548.
- ↑ Weiss HR, Goodall D (2008). "Rate of complications in scoliosis surgery - a systematic review of the Pub Med literature". Scoliosis 3: 9. doi:10.1186/1748-7161-3-9. PMID 18681956.
- ↑ Hawes MC, O'Brien JP (2008). "A century of spine surgery: what can patients expect?". Disability and Rehabilitation 30 (10): 808–17. doi:10.1080/09638280801889972. PMID 18432439.
- ↑ Marieb, Elaine Nicpon (1998). Human anatomy & physiology. San Francisco: Benjamin Cummings. ISBN 0-8053-4360-1.
- ↑ Scoliosis Research Society website
|
||||||||||||||||||||||||||||
|
|||||||||||||||||||||||||||||||||