Quinine
 |
|
|---|---|
 |
|
| Systematic (IUPAC) name | |
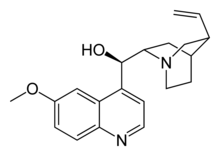
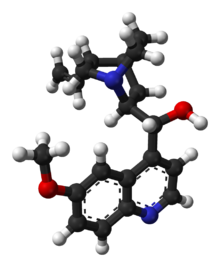
| (R)-(6-methoxyquinolin-4-yl)((2S,4S,8R)- 8-vinylquinuclidin-2-yl)methanol | |
| Identifiers | |
| CAS number | 130-95-0 |
| ATC code | M09AA01 P01BC01 |
| PubChem | CID 8549 |
| DrugBank | DB00468 |
| ChemSpider | 84989 |
| Chemical data | |
| Formula | C20H24N2O2 |
| Mol. mass | 324.417 g/mol |
| Physical data | |
| Melt. point | 177 °C (351 °F) |
| Pharmacokinetic data | |
| Bioavailability | 76 to 88% |
| Protein binding | ~70% |
| Metabolism | Hepatic (mostly CYP3A4 and CYP2C19-mediated) |
| Half-life | ~18 hours |
| Excretion | Renal (20%) |
| Therapeutic considerations | |
| Pregnancy cat. | C (USA), D (Au) |
| Legal status | quinine is now banned in Australia unless specifically for Malaria due to its tendency to kill blood platelets. |
| Routes | Oral, intravenous |
| |
|
Quinine (US: /ˈkwaɪnaɪn/, UK: /ˈkwɪniːn, kwɪˈniːn/) is a natural white crystalline alkaloid having antipyretic (fever-reducing), antimalarial, analgesic (painkilling), anti-inflammatory properties and a bitter taste. It is a stereoisomer of quinidine which, unlike quinine, is an anti-arrhythmic. Quinine contains two major fused-ring systems: the aromatic quinoline and the bicyclic quinuclidine.
Though it has been synthesized in the lab, the bark of the cinchona tree is the only known natural source of quinine. The medicinal properties of the cinchona tree were originally discovered by the Quechua Indians of Peru and Bolivia; later, the Jesuits were the first to bring the cinchona to Europe.
Quinine was the first effective treatment for malaria caused by Plasmodium falciparum, appearing in therapeutics in the 17th century. It remained the antimalarial drug of choice until the 1940s, when other drugs replaced it. Since then, many effective antimalarials have been introduced, although quinine is still used to treat the disease in certain critical situations. Quinine is available with a prescription in the United States and over-the-counter, in very small quantities, in tonic water. Quinine is also used to treat lupus and arthritis. Until recently, quinine was also a common "off-label" treatment for nocturnal leg cramps. This practice is now considered dubious by the FDA[1]
Quinine is very sensitive to ultraviolet light (UV) and will fluoresce in direct sunlight, due to its highly conjugated resonance structure (See Quinoline)
Contents |
Mechanism of action against P. falciparum
As with other quinoline anti-malarial drugs, the action of quinine has not been fully resolved. The most widely accepted hypothesis of quinine action is based on the well-studied and closely related quinoline drug, chloroquine. This model involves the inhibition of hemozoin biocrystallization, which facilitates the aggregation of cytotoxic heme. Free cytotoxic heme accumulates in the parasites, leading to their death.
History
Quinine is an effective muscle relaxant, long used by the Quechua Indians of Peru to halt shivering due to low temperatures. The Peruvians would mix the ground bark of cinchona trees with sweetened water to offset the bark's bitter taste, thus producing tonic water.
Quinine has been used in unextracted form by Europeans since at least the early 17th century. Quinine was first used to treat malaria in Rome in 1631.[2] During the 17th century, malaria was endemic to the swamps and marshes surrounding the city of Rome. Malaria was responsible for the death of several popes, many cardinals and countless common Roman citizens. Most of the priests trained in Rome had seen malaria victims and were familiar with the shivering brought on by the febrile phase of the disease. The Jesuit brother Agostino Salumbrino (1561–1642), an apothecary by training who lived in Lima, observed the Quechua using the bark of the cinchona tree for that purpose. While its effect in treating malaria (and hence malaria-induced shivering) was unrelated to its effect in controlling shivering from rigors, it was still a successful medicine for malaria. At the first opportunity, Salumbrino sent a small quantity to Rome to test as a malaria treatment. In the years that followed, cinchona bark was known as Jesuit's bark and became one of the most valuable commodities shipped from Peru to Europe.
The form of quinine most effective in treating malaria was found by Charles Marie de La Condamine in 1737. Quinine was isolated and named in 1820 by French researchers Pierre Joseph Pelletier and Joseph Bienaimé Caventou. The name was derived from the original Quechua (Inca) word for the cinchona tree bark, "quina" or "quina-quina", which roughly means "bark of bark" or "holy bark". Prior to 1820, the bark was first dried, ground to a fine powder and then mixed into a liquid (commonly wine) which was then drunk. Large scale use of quinine as a prophylaxis started around 1850.
Quinine also played a significant role in the colonization of Africa by Europeans. It has been said that quinine was the prime reason that Africa ceased to be known as the "white man's grave". A historian has stated that "it was quinine's efficacy that gave colonists fresh opportunities to swarm into the Gold Coast, Nigeria and other parts of west Africa".[3]
To maintain their monopoly on cinchona bark, Peru and surrounding countries began outlawing the export of cinchona seeds and saplings beginning in the early 19th century. The Dutch government persisted in its attempt to smuggle the seeds, and by the 1930s Dutch plantations in Java were producing 22 million pounds of cinchona bark, or 97% of the world's quinine production.[3] During World War II, Allied powers were cut off from their supply of quinine when the Germans conquered Holland and the Japanese controlled the Philippines and Indonesia. The United States, however, had managed to obtain four million cinchona seeds from the Philippines and began operation of cinchona plantations in Costa Rica. Nonetheless, such supplies came too late; tens of thousands of U.S. troops in Africa and the South Pacific died due to the lack of quinine.[3] Despite controlling the supply, the Japanese did not make effective use of quinine, and thousands of Japanese troops in the Southwest Pacific died as a result.[4]
Synthetic quinine
Cinchona trees remain the only economically practical source of quinine. However, under wartime pressure, research towards its synthetic production was undertaken. A formal chemical synthesis was accomplished in 1944 by American chemists R.B. Woodward and W.E. Doering.[5] Since then, several more efficient quinine total syntheses have been achieved,[6] but none of them can compete in economic terms with isolation of the alkaloid from natural sources. The first synthetic organic dye, mauveine, was discovered by William Henry Perkin in 1856 while he was attempting to synthesize quinine.
Dosing and indication
As of 2006, quinine is no longer recommended by the WHO as first line treatment for malaria and should be used only when artemesinins are not available.[7][8][9][10]
Quinine is a basic amine and is therefore always presented as a salt. Various preparations that exist include the hydrochloride, dihydrochloride, sulfate, bisulfate and gluconate. This makes quinine dosing complicated since each of the salts has a different weight.
The following amounts of each form are equal:
- quinine base 100 mg
- quinine bisulfate 169 mg
- quinine dihydrochloride 122 mg
- quinine hydrochloride 111 mg
- quinine sulfate (actually (quinine)2H2SO4∙2H2O) 121 mg
- quinine gluconate 160 mg.
All quinine salts may be given orally or intravenously (IV); quinine gluconate may also be given intramuscularly (IM) or rectally (PR).[11][12] The main problem with the rectal route is that the dose can be expelled before it is completely absorbed; this can be corrected by giving a half dose again.
The IV dose of quinine is 8 mg/kg of quinine base every eight hours; the IM dose is 12.8 mg/kg of quinine base twice daily; the PR dose is 20 mg/kg of quinine base twice daily. Treatment should be given for seven days.
The preparations available in the UK are quinine sulfate (200 mg or 300 mg tablets) and quinine hydrochloride (300 mg/ml for injection). Quinine is not licensed for IM or PR use in the UK. The adult dose in the UK is 600 mg quinine dihydrochloride IV or 600 mg quinine sulfate orally every eight hours. For nocturnal leg cramps, the dosage is 200–300 mg at night.[13]
In the United States, quinine sulfate is commercially available in 324-mg tablets under the brand name Qualaquin; the adult dose is two tablets every eight hours. There is no injectable preparation of quinine licensed in the U.S.: quinidine is used instead.[14][15]
Adverse effects
It is usual for quinine in therapeutic doses to cause cinchonism; in rare cases, it may even cause death (usually by pulmonary edema). The development of mild cinchonism is not a reason for stopping or interrupting quinine therapy and the patient should be reassured. Blood glucose levels and electrolyte concentrations must be monitored when quinine is given by injection. The patient should ideally be in cardiac monitoring when the first quinine injection is given (these precautions are often unavailable in developing countries where malaria is endemic).
Cinchonism is much less common when quinine is given by mouth, but oral quinine is not well tolerated (quinine is exceedingly bitter and many patients will vomit after ingesting quinine tablets): Other drugs such as Fansidar (sulfadoxine (sulfonamide antibiotic) with pyrimethamine) or Malarone (proguanil with atovaquone) are often used when oral therapy is required. Quinine ethyl carbonate is tasteless and odourless,[16] but is only commercially available in Japan. Blood glucose, electrolyte and cardiac monitoring are not necessary when quinine is given by mouth.
Quinine can cause paralysis if accidentally injected into a nerve. It is extremely toxic in overdose, and the advice of a poisons specialist should be sought immediately.
Quinine in some cases can lead to constipation,[17] erectile dysfunction and diarrhea.
The New York Times Magazine described a case, presenting with fever, hypotension, and blood abnormalities mimicking septic shock.[18]
Abortifacient
Despite popular belief, quinine is not an effective abortifacient (in the US, quinine is listed as Pregnancy category D [1]). Pregnant women who take toxic doses of quinine will suffer from renal failure before experiencing any kind of quinine-induced abortion.[19] Indeed, quinine is the only drug recommended by the WHO as firstline treatment for uncomplicated malaria in pregnancy.[20]
Disease interactions
Quinine can cause hemolysis in G6PD deficiency, but again this risk is small and the physician should not hesitate to use quinine in patients with G6PD deficiency when there is no alternative. Quinine can also cause drug-induced immune thrombocytopenic purpura (ITP). Symptoms can be severe enough to require hospitalisation and platelet transfusion, with several cases resulting in death.[21]
Quinine can cause abnormal heart rhythms and should be avoided if possible in patients with atrial fibrillation, conduction defects or heart block.
Quinine can worsen hemoglobinuria, myasthenia gravis and optic neuritis.
Hearing impairment
Some studies have related the use of quinine and hearing impairment, in particular high-frequency loss, but it has not been conclusively established whether such impairment is temporary or permanent.[22]
Regulation by the United States Food and Drug Administration
From 1969 to 1992, the U.S. Food and Drug Administration (FDA) received 157 reports of health problems related to quinine use, including 23 which had resulted in death.[23] In 1994, the FDA banned the use of over-the-counter (OTC) quinine as a treatment for nocturnal leg cramps. Pfizer Pharmaceuticals had been selling the brand name Legatrin for this purpose. Doctors may still prescribe quinine, but the FDA has ordered firms to stop marketing unapproved drug products containing quinine. The FDA is also cautioning consumers about off-label use of quinine to treat leg cramps. Quinine is approved for treatment of malaria, but is also commonly prescribed to treat leg cramps and similar conditions. Because malaria is life-threatening, the risks associated with quinine use are considered acceptable when used to treat that affliction.[24]
Though Legatrin was banned by the FDA for the treatment of leg cramps, drug manufacturer URL Mutual has branded a quinine containing drug named "Qualaquin". Qualaquin is marketed as a treatment for malaria and is only sold in the United States by prescription. In 2004, the CDC reported only 1,347 confirmed cases of malaria in the United States.[25]
Non-medical uses of quinine
In some areas, non-medical use of quinine is regulated. For example, in the United States and in Germany, quinine is limited to between 83-85 parts per million.[26]
Beverages
Quinine is a flavor component of tonic water and bitter lemon. According to tradition, the bitter taste of anti-malarial quinine tonic led British colonials in India to mix it with gin, thus creating the gin and tonic cocktail, which is still popular today in many parts of the world, especially the U.K., United States, Canada, Australia, New Zealand, and Lhasa, Tibet. In France, quinine is an ingredient of an apéritif known as Quinquina or "Cap Corse". In Italy, the traditional flavored wine Barolo Chinato is infused with quinine and local herbs and is served as a digestive. In Canada and Italy, quinine is an ingredient in the carbonated chinotto beverages Brio and San Pellegrino Chinotto. In the United Kingdom, the Scottish company A.G. Barr's uses quinine as an ingredient in the carbonated and caffeinated beverage Irn-Bru. In the United Kingdom, Australia, New Zealand, South Africa and Egypt, quinine is an ingredient in Schweppes and other Indian tonic waters. In Uruguay and Argentina, quinine is an ingredient of a Pepsico Inc. Tonic water named Paso de los Toros. In South Africa, quinine is an ingredient of a Clifton Instant Drink named Chikree produced by Tiger Food Brands. On college campuses around the United States tonic water is added to jello shot recipes to make the shot fluoresce.
Scientific

Because of its relatively constant and well-known fluorescence quantum yield, quinine is also used in photochemistry as a common fluorescence standard.
Quinine (and quinidine) are used as the chiral moiety for the ligands used in sharpless asymmetric dihydroxylation.
Bark of Remijia contains 0.5 - 2 % of quinine. The bark is cheaper than bark of Cinchona and as it has an intense taste, it is used for making tonic water.[27]
Other
Quinine is sometimes used as a cutting agent in street drugs such as cocaine and heroin.[28]
Quinine is used as a treatment for Cryptocaryon irritans (commonly referred to as white spot, crypto or marine ich) infection of marine aquarium fish.[29]
See also
- Pharmacology
- Warburg's Tincture
- Luis Jerónimo de Cabrera, 4th Count of Chinchón and Jesuit's bark, for the story of its introduction into Europe
- Stockwell JR. Aeromedical considerations of malaria prophylaxis with mefloquine hydrochloride. Aviation, Space, and Environmental Medicine 1982; 3(10):1011-3
References
- ↑ http://www.fda.gov/Drugs/DrugSafety/PostmarketDrugSafetyInformationforPatientsandProviders/ucm218202.htm
- ↑ Toovey S (May 2004). "The Miraculous Fever-Tree. The Cure that Changed the World Fiametta Rocco; Harper Collins, San Francisco, 2004, 348 pages, Paperback, ISBN 0-00-6532357". Travel Med Infect Dis 2 (2): 109–10. doi:10.1016/j.tmaid.2004.05.001. PMID 17291968.
- ↑ 3.0 3.1 3.2 Conner, Clifford D. (2005). A People's History of Science: Miners, Midwives, and 'Low Mechanicks'. New York: Nation Books. pp. 95–96. ISBN 1560257482. Also cites Porter, Roy (1998). The Greatest Benefit to Mankind: A Medical History of Humanity. New York: W. W. Norton. pp. 465–466. ISBN 0393046346.
- ↑ Fire in the Sky; Willmott, Barrier and the Javelin.
- ↑ Woodward R, Doering W (1944). "The Total Synthesis of Quinine". J Am Chem Soc 66 (849).
- ↑ Kaufman, Teodoro S.; Rúveda, Edmundo A. (2005). "Die Jagd auf Chinin: Etappenerfolge und Gesamtsiege". Angewandte Chemie, Int. Ed. 117 (6): 876–907. doi:10.1002/ange.200400663.
- ↑ World Health Organization (2006). "Guidelines for the treatment of malaria". World Health Organization. http://apps.who.int/malaria/docs/TreatmentGuidelines2006.pdf. Retrieved 10 August 2009.
- ↑ Dorndorp A, Nosten F, Stepniewska K, et al. (2005). "Artesunate verus quinine for treatment of severe falciparum malaria: a randomised trial". Lancet 366: 717–25. doi:10.1016/S0140-6736(05)67176-0.
- ↑ Reyburn, H; Mtove, G; Hendriksen, I; Von Seidlein, L (2009). "Oral quinine for the treatment of uncomplicated malaria". Brit J Med 339: b2066. doi:10.1136/bmj.b2066. PMID 19622550.
- ↑ Achan J, Tibenderana JK, Kyabayinze D, et al. (2009). "Effectiveness of quinine versus artemether-lumefantrine for treating uncomplicated faciparum malaria in Ugandan children". Brit Med J 338: b2763.
- ↑ Barennes H, et al. (1996). "Efficacy and pharmacokinetics of a new intrarectal quinine formulation in children with Plasmodium falciparum malaria". Brit J Clin Pharmacol 41 (5): 389. doi:10.1046/j.1365-2125.1996.03246.x.
- ↑ Barennes, H.; Balima-Koussoubé, T; Nagot, N; Charpentier, JC; Pussard, E (2006). "Safety and efficacy of rectal compared with intramuscular quinine for the early treatment of moderately severe malaria in children: randomised clinical trial". Brit Med J 332 (7549): 1055–57. doi:10.1136/bmj.332.7549.1055. PMID 16675812.
- ↑ BNF 56: Nocturnal leg cramps Accessed 30/11/2008
- ↑ Center for Disease Control (1991). "Treatment with Quinidine Gluconate of Persons with Severe Plasmodium falciparum Infection: Discontinuation of Parenteral Quinine". Morb Mort Weekly Rep 40 (RR-4): 21–23. http://www.cdc.gov/mmwr/preview/mmwrhtml/00043932.htm. Retrieved 2006-05-06.
- ↑ Magill, A; Panosian, C (2005). "Making Antimalarial Agents Available in the United States". New Engl J Med 353 (4): 335–337. doi:10.1056/NEJMp058167. PMID 16000347.
- ↑ Jamaludin A, Mohamad M, Navaratnam V, et al. (1988). "Relative bioavailability of the hydrochloride, sulphate and ethyl carbonate salts of quinine". Br J Clin Pharmacol 25 (2): 261–3. PMID 3358888.
- ↑ Optically active isomers of quinine and quinidine and their respective biological action Accessed 26/1/2009
- ↑ Sanders, L."Poison Pill", "The New York Times", 4/13/2008.
- ↑ Dannenberg AL; Behal, FJ (1983). "Use of quinine for self-induced abortion". The Southern Medical Journal 76 (7): 846–849. PMID 0038-4348.
- ↑ Yeka A, Achan J, D'Alessandro U, Talisuna AO (2009). "Quinine monotherapy for treating uncomplicated malaria in the era of artemisinin-based combination therapy: an appropriate public health policy?". Lancet Infect Dis 9, (7): 448–452. doi:10.1016/S1473-3099(09)70109-4.
- ↑ "NPS warns on quinine". Auspharm e News, 6 January 2010.
- ↑ Department of Clinical Pharmacology, Huddinge University Hospital, Sweden (1994). "The concentration-effect relationship of quinine-induced hearing impairment". Clin Pharmacol Ther 55 (3): 317–323. doi:10.1038/clpt.1994.32. PMID 8143397.
- ↑ "FDA Orders Stop to Marketing Of Quinine for Night Leg Cramps". FDA Consumer Magazine. Food and Drug Administration. July-August 1995. Archived from the original on 2008-01-15. http://web.archive.org/web/20080115020839/http://www.fda.gov/fdac/departs/695_updates.html. Retrieved 2009-07-31.
- ↑ "FDA Orders Unapproved Quinine Drugs from the Market and Cautions Consumers About Off-Label Use of Quinine to Treat Leg Cramps". United States Food and Drug Administration. 2006-12-11. http://www.fda.gov/NewsEvents/Newsroom/PressAnnouncements/2006/ucm108799.htm. Retrieved 2009-07-31.
- ↑ "Malaria Surveillance - United States, 2004". Center for Disease Control. 2006-11-22. http://www.cdc.gov/mmwr/preview/mmwrhtml/ss5504a2.htm. Retrieved 2009-11-22.
- ↑ Ballestero, JA; Plazas, PV; Kracun, S; Gómez-Casati, ME; Taranda, J; Rothlin, CV; Katz, E; Millar, NS et al.; et al. (2005). "Effects of Quinine, Quinidine, and Chloroquine on α9α10 Nicotinic Cholinergic Receptors". Molecular Pharmacology 68 (3): 822–829. doi:10.1124/mol.105.014431. PMID 15955868.
- ↑ Hobhouse, Henry (2004) (in Czech). Šest rostlin, které změnily svět. Prague: Akademie věd České republiky. pp. 59. ISBN 802001179X.
- ↑ (http://www.justice.gov/dea/programs/forensicsci/microgram/mg1009/mg1009.pdf): Microgram Bulletin, Volume 42, Number 10, October 2009, Page 79. Retrieved 21st Apr 2010
- ↑ (http://www.reefculturemagazine.com.au/cryptocaryon.html): Porritt, M., Cryptocaryon irritans, Reef Culture Magazine, 1. Retrieved 9th Jul 2009
Additional reading
- Wolff RS, Wirtschafter D, Adkinson C (June 1997). "Ocular quinine toxicity treated with hyperbaric oxygen". Undersea Hyperb Med 24 (2): 131–4. PMID 9171472. http://archive.rubicon-foundation.org/2278. Retrieved 2008-08-13.
- Hobhouse, Henry - Seeds of Change Six Plants that Transformed Mankind C2005 ISBN(10) 1-59376-049-3
External links
- Jesuits' Powder
- From intox databank
- From inchem
- Database file on Quinine from rain-tree.com
- Catalytic Asymmetric Synthesis of Quinine and Quinidine
- Summary article on history of Quinine in Chemical and Engineering News
- Quinine news page - Alcohol and Drugs History Society
|
|||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||