Hypercholesterolemia
| Hypercholesterolemia | |
|---|---|
| Classification and external resources | |
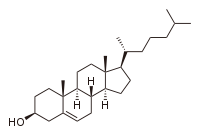 Cholesterol |
|
| ICD-10 | E78.0 |
| ICD-9 | 272.0 |
| DiseasesDB | 6226 |
| eMedicine | med/1073 |
| MeSH | D006937 |
Hypercholesterolemia (literally: high blood cholesterol) is the presence of high levels of cholesterol in the blood.[1] It is not a disease but a metabolic derangement that can be secondary to many diseases and can contribute to many forms of disease, most notably cardiovascular disease. It is closely related to the terms "hyperlipidemia" (elevated levels of lipids) and "hyperlipoproteinemia" (elevated levels of lipoproteins).[1]
Elevated cholesterol in the blood is due to abnormalities in the levels of lipoproteins, the particles that carry cholesterol in the bloodstream. This may be related to diet, genetic factors (such as LDL receptor mutations in familial hypercholesterolemia) and the presence of other diseases such as diabetes and an underactive thyroid. The type of hypercholesterolemia depends on which type of particle (such as low density lipoprotein) is present in excess.[1]
High cholesterol levels are treated with diets low in cholesterol, medications, and rarely with other treatments including surgery (for particular severe subtypes). This has also increased emphasis on other risk factors for cardiovascular disease, such as high blood pressure.[1]
Contents |
Classification
Classically, hypercholesterolemia was categorized by lipoprotein electrophoresis and the Fredrickson classification. Newer methods, such as "lipoprotein subclass analysis" have offered significant improvements in understanding the connection with atherosclerosis progression and clinical consequences.
If the hypercholesterolemia is hereditary (familial hypercholesterolemia), there is more often a family history of premature, earlier onset atherosclerosis, as well as familial occurrence of the signs mentioned above.
Signs and symptoms
Elevated cholesterol does not lead to specific symptoms unless it has been longstanding. Some types of hypercholesterolemia lead to specific physical findings: xanthoma (deposition of cholesterol in patches on the skin or in tendons), xanthelasma palpabrum (yellowish patches around the eyelids) and arcus senilis (white discoloration of the peripheral cornea).[1]
Longstanding elevated hypercholesterolemia leads to accelerated atherosclerosis; this can express itself in a number of cardiovascular diseases: coronary artery disease (angina pectoris, heart attacks), stroke and short stroke-like episodes and peripheral vascular disease.[1][2][3]
Causes
There are a number of secondary causes for high cholesterol:
- Diabetes mellitus and metabolic syndrome
- Kidney disease (nephrotic syndrome)
- Hypothyroidism
- Cushing's syndrome
- Anorexia nervosa
- Sleep deprivation
- Zieve's syndrome
- Family history
- Antiretroviral drugs, like protease inhibitors and nucleoside reverse transcriptase inhibitors.
- Diet
- Body weight
- Physical activity
Diet
While part of the circulating cholesterol originates from diet, and restricting cholesterol intake may reduce blood cholesterol levels, there are various other links between the dietary pattern and cholesterol levels. The American Heart Association compiles a list of the acceptable and unacceptable foods for those who are diagnosed with hypercholesterolemia.
Dietary changes can potentially be very strong: when a group of Tarahumara Indians from Mexico with no obesity or cholesterol problems were exposed to a Western diet, their risk profile worsened significantly, with cholesterol levels rising over thirty percent.[4]
Carbohydrates
Evidence is accumulating that eating more carbohydrates - especially simpler, more refined carbohydrates - increases levels of triglycerides in the blood, lowers HDL, and may shift the LDL particle distribution pattern into unhealthy atherogenic patterns. [5]
Trans fats
An increasing number of researchers are suggesting that a major dietary risk factor for cardiovascular diseases is trans fatty acids, and in the US the FDA has revised food labeling requirements to include listing trans fat quantities.[6]
Diagnosis
There is no specific level at which cholesterol levels are abnormal. Cholesterol levels are found in a continuum within a population. Higher cholesterol levels lead to increased risk of several diseases, most notably cardiovascular diseases. Specifically, high levels of small LDL cholesterol particles are associated with increased risk of heart disease.[7][8] Larger LDL particles do not carry the same risk.
When measuring cholesterol, it is important to measure its subfractions before drawing a conclusion as to the cause of the problem. The subfractions are LDL, HDL and VLDL. In the past, LDL and VLDL levels were rarely measured directly due to cost concerns. VLDL levels are reflected in the levels of triglycerides (generally about 45% of triglycerides is composed of VLDL). LDL was usually estimated as a calculated value from the other fractions (total cholesterol minus HDL and VLDL); this method is called the Friedewald calculation; to be specific: LDL ~= Total Cholesterol - HDL - (0.2 x Triglycerides).
Less expensive (and less accurate) laboratory methods and the Friedewald calculation have long been used because of the complexity, labor, and expense of the electrophoretic methods developed in the 1970s to identify the different lipoprotein particles that transport cholesterol in the blood. In 1980, the original methods, developed by research work in the mid-1970s cost about $5,000, in US 1980 dollars, per blood sample/person.
With time, more advanced laboratory analyses that do measure LDL and VLDL particle sizes and levels have been developed, and at far lower cost. These have partly been developed and become more popular as a result of the increasing clinical trial evidence that intentionally changing cholesterol transport patterns, including to certain abnormal values compared to most adults, often has a dramatic effect on reducing, even partially reversing, the atherosclerotic process. With ongoing research and advances in laboratory methods, the prices for more sophisticated analyses have markedly decreased, to less than $100, US 2004, by some labs, and with simultaneous increases in the accuracy of measurement for some of the methods.
Screening
Screening for a disease refers to testing for a disease, such as hypercholesterolemia, in patients who have no signs or symptoms of the disease.
In patients without any other risk factors, moderate hypercholesterolemia is often not treated. According to Framingham Heart Study, people with an age greater than 50 years have no increased overall mortality with either high or low serum cholesterol levels. There is, however, a correlation between falling cholesterol levels over the first 14 years and mortality over the following 18 years (11% overall and 14% CVD death rate increase per 1 mg/dL per year drop in cholesterol levels). This, however, does not mean that a decrease in serum levels is dangerous, as there has not yet been a recorded heart attack in the study in a person with a total cholesterol below 150 mg/dL.
The U.S. Preventive Services Task Force (USPSTF) has evaluated screening for hypercholesterolemia.[9][10]
Treatment
Clinical Evidence has summarized treatment for both primary prevention[11] and secondary prevention.[12] Two factors have been put forward for consideration when choosing therapy are the patient's risk of coronary disease and their lipoprotein pattern.
- Risk of coronary disease. To calculate the benefit of treatment, there are two online calculators that can estimate baseline risk.[13][14] Combining the baseline risk with the relative risk reduction of a treatment can lead to the absolute risk reduction of number needed to treat. For example, one of the calculators projects that a patient had a 10% risk of coronary disease over ten years. As noted below, the relative risk reduction of a statin is 30%. Thus, after 4–7 years of treatment with a statin, a patient's risk will drop to 7%. This equates to an absolute risk reduction of 3%, or a number needed to treat of 33. Thirty three such patients must be treated for 4–7 years for one to benefit.
- Lipoprotein patterns. (See hyperlipoproteinemia for details) The treatment depends on the type of hypercholesterolemia. Clinical trials, starting in the 1970s, have repeatedly and increasingly found that normal cholesterol values do not necessarily reflect healthy cholesterol values. This has increasingly lead to the newer concept of dyslipidemia, despite normo-cholesterolemia. Thus there has been increasing recognition of the importance of "lipoprotein subclass analysis" as an important approach to better understand and change the connection between cholesterol transport and atherosclerosis progression. Fredrickson Types IIa and IIb can be treated with diet, statins (most prominently rosuvastatin, atorvastatin, simvastatin, or pravastatin), cholesterol absorption inhibitors (ezetimibe), fibrates (gemfibrozil, bezafibrate, fenofibrate or ciprofibrate), vitamin B3 (niacin), bile acid sequestrants (colestipol, cholestyramine), LDL apheresis and in hereditary severe cases liver transplantation.
Diet
In strictly controlled surroundings, such as a hospital ward dedicated to metabolism problems, a diet can reduce cholesterol levels by 15%. In practice, dietary advice can provide a modest decrease in cholesterol levels and may be sufficient in the treatment of mildly elevated cholesterol.[15]
Medications
According to various resources, statins are the most commonly used and effective forms of medication for the treatment of high cholesterol. The U.S. Preventive Services Task Force (USPSTF) estimated that after 5 to 7 years of treatment, the relative risk reduction by statins on coronary heart disease events is decreased by approximately 30%.[9][10] More recently, a meta-analysis reported an almost identical relative risk reduction of 29.2% in low risk patients treated for 4.3 years.[16] A relative risk reduction of 19% in coronary mortality was found in a meta-analysis of patients at all levels of risk.[17]
Clinical practice guidelines
Various clinical practice guidelines have addressed the treatment of hypercholesterolemia. The American College of Physicians has addressed hypercholesterolemia in patients with diabetes.[18] Their recommendations are:
- Recommendation 1: Lipid-lowering therapy should be used for secondary prevention of cardiovascular mortality and morbidity for all patients (both men and women) with known coronary artery disease and type 2 diabetes.
- Recommendation 2: Statins should be used for primary prevention against macrovascular complications in patients (both men and women) with type 2 diabetes and other cardiovascular risk factors.
- Recommendation 3: Once lipid-lowering therapy is initiated, patients with type 2 diabetes mellitus should be taking at least moderate doses of a statin (the accompanying evidence report states "simvastatin, 40 mg/d; pravastatin, 40 mg/d; lovastatin, 40 mg/d; atorvastatin, 20 mg/d; or an equivalent dose of another statin")[19].
- Recommendation 4: For those patients with type 2 diabetes who are taking statins, routine monitoring of liver function tests or muscle enzymes is not recommended except in specific circumstances.
The National Cholesterol Education Program revised their guidelines[20]; however, their 2004 revisions have been criticized for use of nonrandomized, observational data.[21]
In the UK, the National Institute for Health and Clinical Excellence (NICE) has made recommendations for the treatment of elevated cholesterol levels, published in 2008.[22]
Alternative medicine
A survey released in May 2004 by the National Center for Complementary and Alternative Medicine focused on who used complementary and alternative medicine (CAM), what was used, and why it was used in the United States by adults age 18 years and over during 2002. According to this survey, CAM was used to treat cholesterol by 1.1% of U.S. adults who used CAM during 2002 ([1] table 3 on page 9). Consistent with previous studies, this study found that the majority of individuals (i.e., 54.9%) used CAM in conjunction with conventional medicine (page 6).
A review of 84 clinical trials with phytosterols and/or phytostanols reported an average of 8.8% lowering of LDL-cholesterol with a mean daily intake of 2.15 grams/day, administered 2-3 times a day with meals. The dose:response figure shows that more than half of the response is achieved once intake is more than 1.0 g/day.[23] In 2000 the Food and Drug Administration approved a Qualified Health Claim for labeling of foods containing specified amounts of phytosterol esters or phytostanol esters as cholesterol lowering; in 2003 an FDA Interim Health Claim Rule extended that label claim to foods or dietary supplements delivering more than 0.8 grams/day of either esterified or non-esterified ("free") phytosterols or phytostanols divided over two doses per day. Some researchers, however, are concerned about diet supplementation with plant sterol esters and draw attention to significant safety issues. This is why Health Canada, the federal department responsible for helping Canadians maintain and improve their health, has not allowed these foods to be sold in Canada.[24]
Research
Multiple clinical trials, each, by design, examining only one of multiple relevant issues, have increasingly examined the connection between these issues and atherosclerosis clinical consequences. Some of the better recent randomized human outcome trials include ASTEROID, ASCOT-LLA, REVERSAL, PROVE-IT, CARDS, Heart Protection Study, HOPE, PROGRESS, COPERNICUS, and especially a newer research approach utilizing a synthetically produced and IV administered human HDL, the Apo A-I Milano Trial,[25][26][27][28] the results of which were published in JAMA in 2003.
References
- ↑ 1.0 1.1 1.2 1.3 1.4 1.5 Durrington P (2003). "Dyslipidaemia". Lancet 362 (9385): 717–31. doi:10.1016/S0140-6736(03)14234-1. PMID 12957096.
- ↑ Grundy SM, Balady GJ, Criqui MH, et al. (19 May 1998). "Primary prevention of coronary heart disease: guidance from Framingham: a statement for healthcare professionals from the AHA Task Force on Risk Reduction. American Heart Association". Circulation 97 (18): 1876–87. PMID 9603549. http://circ.ahajournals.org/cgi/content/full/97/18/1876.
- ↑ http://labrador.eu/peripheral_vascular_disease_en.html
- ↑ McMurry MP, Cerqueira MT, Connor SL, Connor WE (1991). "Changes in lipid and lipoprotein levels and body weight in Tarahumara Indians after consumption of an affluent diet". N. Engl. J. Med. 325 (24): 1704–8. PMID 1944471. http://content.nejm.org/cgi/content/abstract/325/24/1704.
- ↑ TJ Starc, S Shea, LC Cohn, L Mosca, WM Gersony and RJ Deckelbaum (1998). "Greater dietary intake of simple carbohydrate is associated with lower concentrations of high-density-lipoprotein cholesterol in hypercholesterolemic children". American Journal of Clinical Nutrition 67: 1147–1154. http://www.ajcn.org/cgi/content/abstract/67/6/1147.
- ↑ Mozaffarian D, Katan MB, Ascherio A, Stampfer MJ, Willett WC (April 2006). "Trans fatty acids and cardiovascular disease". N. Engl. J. Med. 354 (15): 1601–13. doi:10.1056/NEJMra054035. PMID 16611951.
- ↑ Girard-Mauduit S (March 2010). "The lipid triad, or how to reduce residual cardiovascular risk?". Ann Endocrinol (Paris). doi:10.1016/j.ando.2010.02.001. PMID 20303470.
- ↑ "The New Blood Lipid Tests -- Sizing Up LDL Cholesterol". Johns Hopkins Medicine. 13 June 2008. http://www.johnshopkinshealthalerts.com/reports/heart_health/1886-1.html.
- ↑ 9.0 9.1 Pignone M, Phillips C, Atkins D, Teutsch S, Mulrow C, Lohr K (2001). "Screening and treating adults for lipid disorders". Am J Prev Med 20 (3 Suppl): 77–89. doi:10.1016/S0749-3797(01)00255-0. PMID 11306236.
- ↑ 10.0 10.1 U.S. Preventive Services Task Force. "Screening for Lipid Disorders: Recommendations and Rationale". http://www.ahrq.gov/clinic/ajpmsuppl/lipidrr.htm. Retrieved February 26, 2007.
- ↑ Pignone M (2005). "Primary prevention: dyslipidaemia". Clin Evid (14): 142–50. PMID 16620402. http://clinicalevidence.com/ceweb/conditions/cvd/0215/0215.jsp.
- ↑ Gami A (2006). "Secondary prevention of ischaemic cardiac events". Clin Evid (15): 195–228. PMID 16973010. http://clinicalevidence.com/ceweb/conditions/cvd/0206/0206_guidelines.jsp.
- ↑ Pignone MP; Sheridan SL. "med-decisions.com". http://www.med-decisions.com/. Retrieved February 26, 2007.
- ↑ National Cholesterol Education Program. "10-year CVD Risk Calculator (Risk Assessment Tool for Estimating 10-year Risk of Developing Hard CHD (Myocardial Infarction and Coronary Death) Version)". http://hp2010.nhlbihin.net/atpiii/calculator.asp?usertype=prof. Retrieved February 26, 2007.
- ↑ Tang JL, Armitage JM, Lancaster T, Silagy CA, Fowler GH, Neil HA (April 1998). "Systematic review of dietary intervention trials to lower blood total cholesterol in free-living subjects". BMJ 316 (7139): 1213–20. PMID 9552999. PMC 28525. http://www.bmj.com/cgi/content/abstract/316/7139/1213.
- ↑ Thavendiranathan P, Bagai A, Brookhart M, Choudhry N (2006). "Primary prevention of cardiovascular diseases with statin therapy: a meta-analysis of randomized controlled trials". Arch Intern Med 166 (21): 2307–13. doi:10.1001/archinte.166.21.2307. PMID 17130382.
- ↑ Baigent C, Keech A, Kearney PM, et al. (2005). "Efficacy and safety of cholesterol-lowering treatment: prospective meta-analysis of data from 90,056 participants in 14 randomised trials of statins". Lancet 366 (9493): 1267–78. doi:10.1016/S0140-6736(05)67394-1. PMID 16214597.
- ↑ Snow V, Aronson M, Hornbake E, Mottur-Pilson C, Weiss K (20 April 2004). "Lipid control in the management of type 2 diabetes mellitus: a clinical practice guideline from the American College of Physicians". Ann Intern Med 140 (8): 644–9. PMID 15096336. http://www.annals.org/cgi/content/full/140/8/644.
- ↑ Vijan S, Hayward RA (2004). "Pharmacologic lipid-lowering therapy in type 2 diabetes mellitus: background paper for the American College of Physicians". Ann. Intern. Med. 140 (8): 650–8. PMID 15096337. http://www.annals.org/cgi/content/full/140/8/650.
- ↑ Grundy SM, Cleeman JI, Merz CN, Brewer HB, Clark LT, Hunninghake DB, Pasternak RC, Smith SC, Stone NJ (2004). "Implications of recent clinical trials for the National Cholesterol Education Program Adult Treatment Panel III Guidelines". J. Am. Coll. Cardiol. 44 (3): 720–32. doi:10.1016/j.jacc.2004.07.001. PMID 15358046.
- ↑ Hayward RA, Hofer TP, Vijan S (2006). "Narrative review: lack of evidence for recommended low-density lipoprotein treatment targets: a solvable problem". Ann. Intern. Med. 145 (7): 520–30. PMID 17015870.
- ↑ National Institute for Health and Clinical Excellence. Clinical guideline 67: Lipid modification. London, May 2008.
- ↑ http://www.ncbi.nlm.nih.gov/pubmed/19091798
- ↑ Weingärtner O. et al. Controversial role of plant sterol esters in the management of hypercholesterolaemia. European Heart Journal 2009 30(4):404-409; doi:10.1093/eurheartj/ehn580. http://eurheartj.oxfordjournals.org/cgi/content/extract/30/4/404
- ↑ url=http://jama.ama-assn.org/cgi/content/full/290/17/2292
- ↑ url=http://www.lipidsonline.org/commentaries/al_abstract.cfm?abs_id=abs047
- ↑ url=http://content.onlinejacc.org/cgi/content/short/44/7/1436
- ↑ url=http://www.lipidsonline.org/commentaries/ppt/milano.ppt
See also
- Familial hypercholesterolemia
|
||||||||||||||||||||||||||||