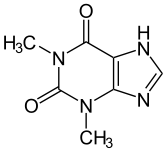
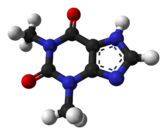
Theophylline
 |
|
|---|---|
 |
|
| Systematic (IUPAC) name | |
| 1,3-dimethyl-7H-purine-2,6-dione | |
| Identifiers | |
| CAS number | 58-55-9 |
| ATC code | R03DA04 |
| PubChem | CID 2153 |
| IUPHAR ligand | 413 |
| DrugBank | DB00277 |
| ChemSpider | 2068 |
| Chemical data | |
| Formula | C7H8N4O2 |
| Mol. mass | 180.164 g/mol |
| SMILES | eMolecules & PubChem |
| Pharmacokinetic data | |
| Bioavailability | 100% |
| Protein binding | 40%, primarily to albumin |
| Metabolism | hepatic to 1-methyluric acid |
| Half-life | 5-8 hours |
| Therapeutic considerations | |
| Pregnancy cat. | A(AU) C(US) |
| Legal status | P (UK) ℞-only (US) |
| Routes | oral, IV |
| |
|

Theophylline, also known as dimethylxanthine, is a methylxanthine drug used in therapy for respiratory diseases such as COPD and asthma under a variety of brand names. Because of its numerous side-effects, the drug are now rarely administered for clinical use. As a member of the xanthine family, it bears structural and pharmacological similarity to caffeine. It is naturally found in tea, although in trace amounts (~1 mg/L),[1] significantly less than therapeutic doses.[2] It is found also in cocoa beans. Amounts as high as 3.7 mg/g have been reported in Criollo cocoa beans.[3]
The main actions of theophylline involve:
- relaxing bronchial smooth muscle
- increasing heart muscle contractility and efficiency: positive inotropic
- increasing heart rate: positive chronotropic
- increasing blood pressure
- increasing renal blood flow
- some anti-inflammatory effects
- central nervous system stimulatory effect mainly on the medullary respiratory center.
Contents |
History
Theophylline was first extracted from tea leaves and chemically identified around 1888 by the German biologist Albrecht Kossel.[4][5] Just seven years after its discovery, a chemical synthesis starting with 1,3-dimethyluric acid was described by Emil Fischer and Lorenz Ach.[6] The Traube synthesis, an alternative method to synthesize Theophylline has been introduced in 1900 by another German scientist, Wilhelm Traube.[7] Theophylline's first clinical use came in 1902 as diuretic.[8] It took an additional 20 years until its first description in asthma treatment.[9]
Pharmacokinetics
Absorption
Bioavailability is 100%. However, taking the drug late in the evening may slow the absorption process, without affecting the bioavailability. Taking the drug after a meal high in fat content will also slow down the absorption process, without affecting the bioavailability.
Distribution
Theophylline is distributed in the extracellular fluid, in the placenta, in the mother's milk and in the central nervous system. The volume of distribution is 0.5 L/kg. The protein binding is 40%. The volume of distribution may increase in neonates and those suffering from cirrhosis or malnutrition, whereas the volume of distribution may decrease in those suffering from obesity.
Metabolism
Theophylline is metabolized extensively in the liver (up to 70%). It undergoes N-demethylation via cytochrome P450 1A2. It is metabolized by parallel first order and Michaelis-Menten pathways. Metabolism may become saturated (non-linear), even within the therapeutic range. Small dose increases may result in disproportionately large increases in serum concentration. Methylation in caffeine is also important in the infant population. Smokers and people with hepatic (liver) impairment metabolize it differently.
Elimination
Theophylline is excreted unchanged in the urine (up to 10%). Clearance of the drug is increased in these conditions: children 1 to 12, teenagers 12 to 16, adult smokers, elderly smokers, cystic fibrosis, hyperthyroidism. Clearance of the drug is decreased in these conditions: elderly, acute congestive heart failure, cirrhosis, hypothyroidism and febrile viral illness.
The elimination half-life varies: 30 hours for premature neonates, 24 hours for neonates, 3.5 hours for children ages 1 to 9, 8 hours for adult non-smokers, 5 hours for adult smokers, 24 hours for those with hepatic impairment, 12 hours for those with congestive heart failure NYHA class I-II, 24 hours for those with congestive heart failure NYHA class III-IV, 12 hours for the elderly.
Indications
The main therapeutic uses of theophylline are aimed at:
Uses Under Investigation
A clinical study reported in 2008 that theophylline was helpful in improving the sense of smell in study subjects with anosmia.[10]
Mechanisms of action
Like other methylated xanthine derivatives, theophylline is both a
- competitive nonselective phosphodiesterase inhibitor, [11] which raises intracellular cAMP, activates PKA, inhibits TNF-alpha [12] [13] and inhibits leukotriene [14] synthesis, and reduces inflammation and innate immunity [14]
- nonselective adenosine receptor antagonist [15], antagonizing A1, A2, and A3 receptors almost equally, which explains many of its cardiac effects and some of its anti-asthmatic effects.
Theophylline has been shown to inhibit TGF-beta-mediated conversion of pulmonary fibroblasts into myofibroblasts in COPD and asthma via cAMP-PKA pathway and suppresses COL1 mRNA, which codes for the protein collagen.[16]
It has been shown that theophylline may reverse the clinical observations of steroid insensitivity in patients with COPD and asthmatics that are active smokers (a condition resulting in oxidative stress) via a distinctly separate mechanism. Theophylline in vitro can restore the reduced HDAC (histone deacetylase) activity that is induced by oxidative stress (i.e., in smokers), returning steroid responsiveness toward normal.[17] Furthermore, theophylline has been shown to directly activate HDAC2.[18] (Corticosteroids switch off the inflammatory response by blocking the expression of inflammatory mediators through deacetylation of histones, an effect mediated via histone deacetylase-2 (HDAC2). Once deacetylated, DNA is repackaged so that the promoter regions of inflammatory genes are unavailable for binding of transcription factors such as NF-κB that act to turn on inflammatory activity. It has recently been shown that the oxidative stress associated with cigarette smoke can inhibit the activity of HDAC2, thereby blocking the anti-inflammatory effects of corticosteroids.) Thus theophylline could prove to be a novel form of adjunct therapy in improving the clinical response to steroids in smoking asthmatics.
Side-effects
The use of theophylline is complicated by the fact that it interacts with various drugs, chiefly cimetidine and phenytoin, and that it has a narrow therapeutic index, so its use must be monitored to avoid toxicity. It can also cause nausea, diarrhea, increase in heart rate, arrhythmias, and CNS excitation (headaches, insomnia, irritability, dizziness and lightheadedness).[19][20] Seizures can also occur in severe cases of toxicity and is considered to be a neurological emergency.[21] Its toxicity is increased by erythromycin, cimetidine, and fluoroquinolones, such as ciprofloxacin. It can reach toxic levels when taken with fatty meals, an effect called dose dumping.[22]
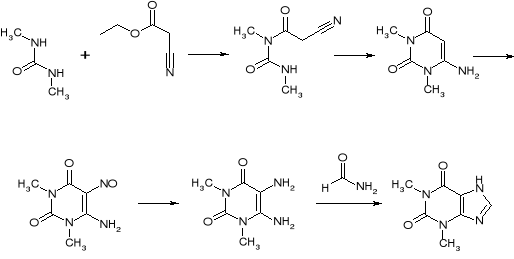
Synthesis
Theophylline can be prepared synthetically starting from dimethylurea and ethyl 2-cyanoacetate.
References
- ↑ MAFF Food Surveillance Information Sheet
- ↑ RXlist dosage and administration information for theophylline
- ↑ Apgar, Joan L.; Tarka, Jr., Stanly M. (1998). "Methylxanthine composition and consumption patterns of cocoa and chocolate products". In Gene A. Spiller. Caffeine. CRC Press. p. 171. ISBN 0849326478. http://books.google.com/?id=WxmBmvhsoZ8C&pg=PA171
- ↑ Kossel A. (1888). "Über eine neue Base aus dem Pflanzenreich.". Ber. Dtsch. Chem. Ges. 21: 2164–2167. doi:10.1002/cber.188802101422..
- ↑ Kossel A. (1889). "Über das Theophyllin, einen neuen Bestandtheil des Thees.". Hoppe Seylers Z. Physiol. Chem. 13: 298–308..
- ↑ Fischer E., Ach L. (1895). "Synthese des Caffeins.". Ber. Dtsch. Chem. Ges. 28: 3139..
- ↑ Traube W (1900). "Der synthetische Aufbau der Harnsäure, des Xanthins, Theobromins, Theophyllins und Caffeïns aus der Cyanessigsäure]". Chem. Ber. 33: 3035–3056. doi:10.1002/cber.19000330352.
- ↑ Minkowski O. (1902). "Über Theocin (Theophyllin) als Diureticum.". Ther. Gegenwart 43: 490–493..
- ↑ Schultze-Werninghaus G., Meier-Sydow J. (1982). "The clinical and pharmacological history of theophylline: first report on the bronchospasmolytic action in man by S. R. Hirsch in Frankfurt (Main) 1922.". Clin. Allergy 12 (2): 211–215. doi:10.1111/j.1365-2222.1982.tb01641.x. PMID 7042115..
- ↑ For Some Who Have Lost Their Sense Of Smell, A Once Popular Asthma Drug Could Help. Science Daily, American Physiological Society
- ↑ Essayan DM. (2001). "Cyclic nucleotide phosphodiesterases.". J Allergy Clin Immunol. 108 (5): 671–80. doi:10.1067/mai.2001.119555. PMID 11692087.
- ↑ Deree J, Martins JO, Melbostad H, Loomis WH, Coimbra R. (2008). "Insights into the regulation of TNF-alpha production in human mononuclear cells: the effects of non-specific phosphodiesterase inhibition.". Clinics (Sao Paulo). 63 (3): 321–8. doi:10.1590/S1807-59322008000300006. PMID 18568240.
- ↑ Marques LJ, Zheng L, Poulakis N, Guzman J, Costabel U (February 1999). "Pentoxifylline inhibits TNF-alpha production from human alveolar macrophages". Am. J. Respir. Crit. Care Med. 159 (2): 508–11. PMID 9927365. http://ajrccm.atsjournals.org/cgi/pmidlookup?view=long&pmid=9927365.
- ↑ 14.0 14.1 Peters-Golden M, Canetti C, Mancuso P, Coffey MJ. (2005). "Leukotrienes: underappreciated mediators of innate immune responses.". J Immunol. 174 (2): 589–94. PMID 15634873. http://www.jimmunol.org/cgi/content/full/174/2/589.
- ↑ Daly JW, Jacobson KA, Ukena D. (1987). "Adenosine receptors: development of selective agonists and antagonists.". Prog Clin Biol Res. 230 (1): :41–63. PMID 3588607.
- ↑ Yano, Biochem and Biophys Res Comm V341-3, 2006
- ↑ Ito et al., 2002a
- ↑ Ito et al., 2002b
- ↑ MedlinePlus Drug Information: Theophylline
- ↑ THEOPHYLLINE - ORAL 24 HOUR TABLET (Uni-Dur) side effects, medical uses, and drug interactions
- ↑ Yoshikawa, H. (Apr 2007). "First-line therapy for theophylline-associated seizures.". Acta Neurol Scand 115 (4 Suppl): 57–61. doi:10.1111/j.1600-0404.2007.00810.x. PMID 17362277.
- ↑ Food-induced "dose-dumping" from a once-a-day theophylline product as a cause of theophylline toxicity.
|
|||||||||||||||||||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||