Diverticulitis
| Diverticulitis | |
|---|---|
| Classification and external resources | |
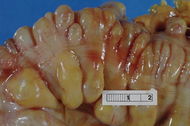 Large bowel (sigmoid colon) showing multiple diverticula. The diverticula appear on either side of the longitudinal muscle bundle (taenium). |
|
| ICD-10 | K57. |
| ICD-9 | 562 |
| DiseasesDB | 3876 |
| MedlinePlus | 000257 |
| eMedicine | med/578 |
| MeSH | D004238 |
Diverticulitis is a common digestive disease particularly found in the large intestine. Diverticulitis develops from diverticulosis, which involves the formation of pouches (diverticula) on the outside of the colon. Diverticulitis results if one of these diverticula becomes inflamed.
Contents |
Signs and symptoms
Patients often present with the classic triad of left lower quadrant pain, fever, and leukocytosis (an elevation of the white cell count in blood tests). Patients may also complain of nausea or diarrhea; others may be constipated.
Less commonly, an individual with diverticulitis may present with right-sided abdominal pain. This may be due to the less prevalent right-sided diverticula or a very redundant sigmoid colon.
Diverticulitis
The most common symptom of diverticulitis is abdominal pain. The most common sign is tenderness around the left side of the lower abdomen. If infection is the cause, then nausea, vomiting, feeling hot while having no fever, cramping, and constipation may occur as well. The severity of symptoms depends on the extent of the infection and complications. Diverticulitis worsens throughout the day, as it starts as small pains and slowly turns into vomiting and sharp pains.
Diverticulosis
Most people with diverticulosis do not have any discomfort or symptoms; however, symptoms may include mild cramps, bloating, and constipation. Other diseases such as inflammatory bowel disease (IBD) and stomach ulcers cause similar problems, so these symptoms do not always mean a person has diverticulosis.
Causes
The development of colonic diverticulum is thought to be a result of raised intraluminal colonic pressures. The sigmoid colon (Section 4) has the smallest diameter of any portion of the colon, and therefore the portion which would be expected to have the highest intraluminal pressure. The claim that a lack of dietary fiber, particularly non-soluble fiber (also known in older parlance as "roughage") predisposes individuals to diverticular disease is supported within the medical literature.[1][2]
Diet
Peanuts and seeds were, in the past, thought by many health care professionals to possibly aggravate diverticulitis.[3] However, recent studies have found no evidence that suggests the avoidance of nuts and seeds prevents the progression of diverticulosis to an acute case of diverticulitis.[4][5]
Popcorn, nuts and corn were also not recommended in the past for diverticulitis patients. Recent research has shown that not only they don't seem to be causing more diverticulitis or worsening it, but a higher intake of nuts and corn could be helping to avoid diverticulitis in grown men.[6]
Diagnosis
People with the above symptoms are commonly studied with a computed tomography, or CT scan.[7] The CT scan is very accurate (98%) in diagnosing diverticulitis. In order to extract the most information possible about the patient's condition, thin section (5mm) transverse images are obtained through the entire abdomen and pelvis after the patient has been administered oral and intravascular contrast. Images reveal localized thickening and hyperemia (increased blood flow) involving a segment of the colon wall, with inflammatory changes extending into the fatty tissues surrounding the colon. The diagnosis of acute diverticulitis is made confidently when the involved segment contains diverticulae.[8] CT may also identify patients with more complicated diverticulitis, such as those with an associated abscess. It may even allow for radiologically guided drainage of an associated abscess, sparing a patient from immediate surgical intervention.
Other studies, such as barium enema and colonoscopy are contraindicated in the acute phase of diverticulitis due to the risk of perforation.
Differential diagnosis
The differential diagnosis includes colon cancer, inflammatory bowel disease, ischemic colitis, and irritable bowel syndrome, as well as a number of urological and gynecological processes. Some patients report bleeding from the rectum.
Treatment
An initial episode of acute diverticulitis is usually treated with bowel rest (i.e., nothing by mouth), IV fluid resuscitation, and broad-spectrum antibiotics which cover anaerobic bacteria and gram-negative rods. However, recurring acute attacks or complications, such as peritonitis, abscess, or fistula may require surgery, either immediately or on an elective basis.
Upon discharge patients may be placed on a low residue diet.[9] This low-fiber diet gives the colon adequate time to heal without needing to be overworked. Later, patients are placed on a high-fiber diet.
In some cases surgery may be required to remove the area of the colon with the diverticula. Patients suffering their first attack of diverticulitis are typically not encouraged to undergo the surgery, unless the case is severe. Patients suffering repeated episodes may benefit from the surgery. In such cases the risks of complications from the diverticulitis outweigh the risks of complications from surgery.
Most cases of simple, uncomplicated diverticulitis respond to conservative therapy with bowel rest and antibiotics.[10]
Surgery
Diverticulitis surgery may be elective or may be a medical emergency. Whether the elective surgery should be performed or not is decided based on several external factors such as the stage of the disease, the age of the patient and his or her general medical condition, as well as the severity and frequency of attacks or if the symptoms persisted after a first acute episode. In most cases, the decision to perform elective surgery is taken when the risks of the surgery are smaller than the ones resulted from the complication of the condition. Elective surgery may be performed at least 6 weeks after recovery from acute diverticulitis.[11]
Emergency surgery is necessary for people whose intestine has ruptured; intestinal rupture always results in infection of the abdominal cavity.[12] During a diverticulitis surgery, the ruptured section is removed and a colostomy is performed. This means that the surgeon will create an opening between the large intestine and the surface of the skin. The colostomy is closed in about 10 or 12 weeks in a different surgery in which the cut ends of the intestine are rejoined.
The first surgical approach consists in the resection and primary anastomosis. This first stage of surgery is performed on patients with a well vascularized, nonedematous and tension-free bowel. The proximal margin should be an area of pliable colon without hypertrophy or inflammation. The distal margin should extend to the upper third of the rectum where the taenia coalesces. Not all of the diverticula-bearing colon must be removed, since diverticula proximal to the descending or sigmoid colon are unlikely to result in further symptoms.[13]
Diverticulitis surgery can be done in two ways: through a primary bowel resection or through a bowel resection with colostomy. Both bowel resections may be done in the traditional way or by laparoscopic surgery.[14] The traditional bowel resection is made using an open surgical approach, called colectomy. During a colectomy, the patient is placed under general anesthesia in order to make sure that the patient will not feel any pain and he or she will be completely asleep during the procedure. A surgeon performing a colectomy will make a lower midline incision in the abdomen or a lateral lower transverse incision. The diseased section of the large intestine is removed and then the two healthy ends are sewn or stapled back together. A colostomy may be performed when the bowel has to be relieved of its normal digestive work as it heals. A colostomy implies creating a temporary opening of the colon on the skin surface and the end of the colon is passed through the abdominal wall and a removable bag is attached to it. The waste will be collected in the bag.[15]
However, most of the surgeons prefer performing the bowel resection laparoscopically mainly because the postoperative pain is reduced and the patient's recovery is faster. The laparoscopic surgery is a minimally invasive procedure in which three to four smaller incisions are made in the abdomen or navel.
All colon surgery involves only three maneuvers that may vary in complexity depending on the region of the bowel and the nature of the disease which are the retraction of the colon, the division of the attachments to the colon and the dissection of the mesentery.[16] After the resection of the colon, the surgeon normally divides the attachments to the liver and the small intestine. After the mesenteric vessels are dissected, the colon is divided with special surgical staplers that close off the bowel while cutting between the staple lines.
Primary Bowel Resection
The primary bowel resection is the standard procedure for patients with diverticulitis. It consists in the removal of the diseased or ruptured part of the intestine which is then reconnected to healthy segments of the colon. This is called anastomosis. Depending on the patient's general medical condition, the procedure may be done traditionally, via a colectomy or laparoscopically, which requires smaller incisions and a faster recovery.[17]
Bowel Resection with Colostomy
This procedure is also known as the Hartmann's operation and it is done when rejoining the colon and rectum is too risky due to the excessive inflammation of the colon. This is a more complicated surgery which is mostly performed in life-threatening cases. The bowel resection with colostomy implies a temporary colostomy which is followed by a second operation which has the purpose to reverse the colostomy. The surgeon makes an opening in the abdominal wall (a colostomy) which helps clearing the infection and inflammation. The colon is brought out through the opening and all waste is collected into an external bag.[18]
However, the colostomy is usually temporary but it may be permanent as well depending on the severity of the case. Most of the time, several months later after the inflammation has healed, the patient undergoes another major surgery during which the surgeon rejoins the colon and rectum and reverses the colostomy.
Complications
In complicated diverticulitis, bacteria may subsequently infect the outside of the colon if an inflamed diverticulum bursts open. If the infection spreads to the lining of the abdominal cavity, (peritoneum), this can cause a potentially fatal peritonitis. Sometimes inflamed diverticula can cause narrowing of the bowel, leading to an obstruction. Also, the affected part of the colon could adhere to the bladder or other organ in the pelvic cavity, causing a fistula, or abnormal connection between an organ and adjacent structure or organ, in this case the colon and an adjacent organ.
- Bowel obstruction
- Peritonitis
- Abscess
- fistula
- Bleeding
- Strictures
Epidemiology
Diverticulitis most often affects middle-aged and elderly persons, though it can strike younger patients as well.[19] Central obesity may be associated with diverticulitis in younger patients, with some being as young as 20 years old.[20]
In Western countries, diverticular disease most commonly involves the sigmoid colon - section 4 - (95% of patients). The prevalence of diverticular disease has increased from an estimated 10% in the 1920s to between 35 and 50% by the late 1960s. 65% of those currently 85 years of age and older can be expected to have some form of diverticular disease of the colon. Less than 5% of those aged 40 years and younger may also be affected by diverticular disease.
Left-sided diverticular disease (involving the sigmoid colon) is most common in the West, while right-sided diverticular disease is more prevalent in Asia and Africa. Among patients with diverticulosis, 10–25% patients will go on to develop diverticulitis within their lifetimes.
References
- ↑ "Diverticular disease". Umm.edu. 2008-08-29. http://www.umm.edu/altmed/articles/diverticular-disease-000051.htm. Retrieved 2010-02-10.
- ↑ "Diverticular Disease: Oregon Health & Science University - Portland, Oregon". Ohsu.edu. http://www.ohsu.edu/health/health-topics/topic.cfm?id=8464. Retrieved 2010-02-10.
- ↑ "Avoid Certain Foods To Prevent Diverticulitis - Health News Story - KNSD". http://www.nbcsandiego.com/health/4963158/detail.html. Retrieved 2007-11-19.
- ↑ "Patient information: Diverticular disease". http://www.uptodate.com/patients/content/topic.do?topicKey=~thW_vUMq.OAM3h&selectedTitle=2~15&source=search_result. Retrieved 2008-02-12.
- ↑ Michael Picco. "Question. Diverticulitis diet: Should I avoid nuts and seeds?". Nutrition and healthy eating. Expert answers.. Mayo clinic. http://www.mayoclinic.com/health/diverticulitis-diet/AN01255.
- ↑ Todd Neale (August 26, 2008). "Nuts and Corn Held Blameless in Diverticular Disease". medpagetoday.com. http://www.medpagetoday.com/Gastroenterology/GeneralGastroenterology/10670. It's citing Lisa L. Strate, Yan L. Liu, Sapna Syngal, Walid H. Aldoori, Edward L. Giovannucci (2008). "Nut, Corn, and Popcorn Consumption and the Incidence of Diverticular Disease". Journal of American Medical Association 300 (8): 907–914. doi:10.1001/jama.300.8.907. PMID 18728264. PMC 2643269. http://jama.ama-assn.org/cgi/content/abstract/300/8/907
- ↑ Lee KH, Lee HS, Park SH, et al (2007). "Appendiceal diverticulitis: diagnosis and differentiation from usual acute appendicitis using computed tomography". Journal of computer assisted tomography 31 (5): 763–9. doi:10.1097/RCT.0b013e3180340991. PMID 17895789.
- ↑ Horton KM et al. (Mar-Apr 2000). "CT Evaluation of the Colon: Inflammatory Disease". Radiographics 20 (2): 399–418. PMID 10715339.
- ↑ Mitchell J. Spirt, MD (January 2010). "Complicated Intra-abdominal Infections: A Focus on Appendicitis and Diverticulitis". Postgraduate Medicine 122 (1): 39–51. doi:10.3810/pgm.2010.01.2098. PMID 20107288. http://www.postgradmed.com/index.php?article=2098.
- ↑ Bogardus, Sydney (Aug 2006). "What do we know about diverticular disease? A brief overview". Journal of Clinical Gastroenterology 40 Supplement 3: S108–11. doi:10.1097/01.mcg.0000212603.28595.5c. PMID 16885691.
- ↑ Merck, Sharpe & Dohme. "Diverticulitis treatments" 2010-02-23.
- ↑ What's the diverticulitis surgery? Digestive Disoders portal. Retrieved on 2010-02-23
- ↑ Diverticulitis: Treatment & Medication eMedicine. 2010-02-23
- ↑ Diverticulitis Surgery 2010-02-23
- ↑ Schein, Moshe (MD). "Diverticulitis surgery treatment" 2010-02-23.
- ↑ Bowel resection procedure Encyclopedia of surgery. Retrieved on 2010-02-23
- ↑ National Center for Biotechnology Information. "Primary bowel resection and diverticulitis" 2010-02-23.
- ↑ Diverticulitis treatments and drugs Mayo Clinic. 2010-02-23
- ↑ Cole CD, Wolfson AB (2007). "Case Series: Diverticulitis in the Young". J Emerg Med 33 (4): 363. doi:10.1016/j.jemermed.2007.02.022. PMID 17976749.
- ↑ "Disease Of Older Adults Now Seen In Young, Obese Adults". http://www.sciencedaily.com/releases/2006/09/060923104630.htm. Retrieved 2007-11-19.
External links
- Health and Disease Information on Diverticulitis at Penn State University
- Diverticulosis and Diverticulitis at NIDDK
- Diverticulitis at Mayo Clinic
|
|||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||