Tetanus
| Tetanus | |
|---|---|
| Classification and external resources | |
 Muscular spasms (specifically opisthotonos) in a patient suffering from tetanus. Painting by Sir Charles Bell, 1809. |
|
| ICD-10 | A33.-A35. |
| ICD-9 | 037, 771.3 |
| DiseasesDB | 2829 |
| MedlinePlus | 000615 |
| eMedicine | emerg/574 |
| MeSH | D013742 |
Tetanus, also called lockjaw, is a medical condition characterized by a prolonged contraction of skeletal muscle fibers. The primary symptoms are caused by tetanospasmin, a neurotoxin produced by the Gram-positive, obligate anaerobic bacterium Clostridium tetani. Infection generally occurs through wound contamination and often involves a cut or deep puncture wound. As the infection progresses, muscle spasms develop in the jaw (thus the name "lockjaw") and elsewhere in the body.[1] Infection can be prevented by proper immunization and by post-exposure prophylaxis.[2]
Contents |
Signs and symptoms

Tetanus affects skeletal muscle, a type of striated muscle used in voluntary movement. The other type of striated muscle, cardiac or heart muscle, cannot be tetanized because of its intrinsic electrical properties. Mortality rates reported vary from 48% to 73%. In recent years, approximately 11% of reported tetanus cases have been fatal. The highest mortality rates are in unvaccinated people and people over 60 years of age.[2]
The incubation period of tetanus may be up to several months but is usually about 8 days.[3][4] In general, the further the injury site is from the central nervous system, the longer the incubation period. The shorter the incubation period, the more severe the symptoms.[5] In neonatal tetanus, symptoms usually appear from 4 to 14 days after birth, averaging about 7 days. On the basis of clinical findings, four different forms of tetanus have been described.[2]
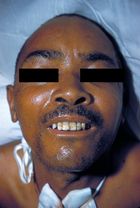
Generalized tetanus is the most common type of tetanus, representing about 80% of cases. The generalized form usually presents with a descending pattern. The first sign is trismus, or lockjaw, and the facial spasms called risus sardonicus, followed by stiffness of the neck, difficulty in swallowing, and rigidity of pectoral and calf muscles. Other symptoms include elevated temperature, sweating, elevated blood pressure, and episodic rapid heart rate. Spasms may occur frequently and last for several minutes with the body shaped into a characteristic form called opisthotonos. Spasms continue for up to 4 weeks, and complete recovery may take months.
Neonatal tetanus is a form of generalized tetanus that occurs in newborns. Infants who have not acquired passive immunity because the mother has never been immunized are at risk. It usually occurs through infection of the unhealed umbilical stump, particularly when the stump is cut with a non-sterile instrument. Neonatal tetanus is common in many developing countries and is responsible for about 14% (215,000) of all neonatal deaths, but is very rare in developed countries.[6]
Local tetanus is an uncommon form of the disease, in which patients have persistent contraction of muscles in the same anatomic area as the injury. The contractions may persist for many weeks before gradually subsiding. Local tetanus is generally milder; only about 1% of cases are fatal, but it may precede the onset of generalized tetanus.
Cephalic tetanus is a rare form of the disease, occasionally occurring with otitis media (ear infections) in which C. tetani is present in the flora of the middle ear, or following injuries to the head. There is involvement of the cranial nerves, especially in the facial area.
Cause
Tetanus is often associated with rust, especially rusty nails, but this concept is somewhat misleading. Objects that accumulate rust are often found outdoors, or in places that harbor anaerobic bacteria, but the rust itself does not cause tetanus nor does it contain more C. tetani bacteria. The rough surface of rusty metal merely provides a prime habitat for a C. tetani endospore to reside, and the nail affords a means to puncture skin and deliver endospore into the wound. An endospore is a non-metabolising survival structure that begins to metabolise and cause infection once in an adequate environment. Because C. tetani is an anaerobic bacterium, it and its endospores survive well in an environment that lacks oxygen. Hence, stepping on a nail (rusty or not) may result in a tetanus infection, as the low-oxygen (anaerobic) environment is provided by the same object which causes a puncture wound, delivering endospores to a suitable environment for growth.
Pathophysiology
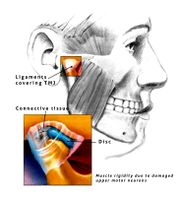
Tetanus begins when spores of Clostridium tetani enter damaged tissue. The spores transform into rod-shaped bacteria and produce the neurotoxin tetanospasmin (also known as tetanus toxin). This toxin is inactive inside the bacteria, but when the bacteria dies, it is released and activated by proteases. Active tetanospasmin is carried by retrograde axonal transport[5][7] to the spinal cord and brain stem where it binds irreversibly to receptors at these sites.[5] It cleaves membrane proteins involved in neuroexocytosis,[8] which in turn blocks neurotransmission. Ultimately, this produces the symptoms of the disease. Damaged upper motor neurons can no longer inhibit lower motor neurons (see Renshaw cells), plus they cannot control reflex responses to afferent sensory stimuli.[5] Both mechanisms produce the hallmark muscle rigidity and spasms. Similarly, a lack of neural control of the adrenal glands results in release of catecholamines, thus producing a hypersympathetic state and widespread autonomic instability.
C. tetani also produces tetanolysin, another toxin whose role in tetanus is unknown.
Diagnosis
There are no blood tests that can be used to diagnose tetanus. The diagnosis is based on the presentation of tetanus symptoms and does not depend upon isolation of the bacteria, which is recovered from the wound in only 30% of cases and can be isolated from patients who do not have tetanus. Laboratory identification of C. tetani can only be demonstrated by production of tetanospasmin in mice.[2]
The "spatula test" is a clinical test for tetanus that involves touching the posterior pharyngeal wall with a sterile, soft-tipped instrument, and observing the effect. A positive test result is the involuntary contraction of the jaw (biting down on the "spatula"), and a negative test result would normally be a gag reflex attempting to expel the foreign object. A short report in The American Journal of Tropical Medicine and Hygiene states that in a patient research study, the spatula test had a high specificity (zero false-positive test results) and a high sensitivity (94% of infected patients produced a positive test result).[9]
Prevention
Unlike many infectious diseases, recovery from naturally acquired tetanus does not usually result in immunity to tetanus. This is due to the extreme potency of the tetanospasmin toxin; even a lethal dose of tetanospasmin is insufficient to provoke an immune response.
Tetanus can be prevented by vaccination with tetanus toxoid.[10] The CDC recommends that adults receive a booster vaccine every ten years[11], and standard care practice in many places is to give the booster to any patient with a puncture wound who is uncertain of when he or she was last vaccinated, or if he or she has had fewer than 3 lifetime doses of the vaccine. The booster may not prevent a potentially fatal case of tetanus from the current wound, however, as it can take up to two weeks for tetanus antibodies to form.[12] In children under the age of seven, the tetanus vaccine is often administered as a combined vaccine, DPT/DTaP vaccine, which also includes vaccines against diphtheria and pertussis. For adults and children over seven, the Td vaccine (tetanus and diphtheria) or Tdap (tetanus, diphtheria, and acellular pertussis) is commonly used.[10]
Treatment
The wound must be cleaned. Dead and infected tissue should be removed by surgical debridement. Administration of the antibiotic metronidazole decreases the number of bacteria but has no effect on the bacterial toxin. Penicillin was once used to treat tetanus, but is no longer the treatment of choice, owing to a theoretical risk of increased spasms. However, its use is recommended if metronidazole is not available. Passive immunization with human anti-tetanospasmin immunoglobulin or tetanus immunoglobulin is crucial. If specific anti-tetanospasmin immunoglobulin is not available, then normal human immunoglobulin may be given instead. All tetanus victims should be vaccinated against the disease or offered a booster shot.
Mild tetanus
Mild cases of tetanus can be treated with:
- Tetanus immunoglobulin IV or IM,
- metronidazole IV for 10 days,
- diazepam,
- tetanus vaccination
Severe tetanus
Severe cases will require admission to intensive care. In addition to the measures listed above for mild tetanus:
- human tetanus immunoglobulin injected intrathecally (increases clinical improvement from 4% to 35%)
- tracheostomy and mechanical ventilation for 3 to 4 weeks,
- magnesium, as an intravenous (IV) infusion, to prevent muscle spasm,
- diazepam as a continuous IV infusion,
- the autonomic effects of tetanus can be difficult to manage (alternating hyper- and hypotension, hyperpyrexia/hypothermia) and may require IV labetalol, magnesium, clonidine, or nifedipine.
Drugs such as diazepam or other muscle relaxants can be given to control the muscle spasms. In extreme cases it may be necessary to paralyze the patient with curare-like drugs and use a mechanical ventilator.
In order to survive a tetanus infection, the maintenance of an airway and proper nutrition are required. An intake of 3500-4000 calories, and at least 150 g of protein per day, is often given in liquid form through a tube directly into the stomach (Percutaneous endoscopic gastrostomy), or through a drip into a vein (Total parenteral nutrition). This high-caloric diet maintenance is required because of the increased metabolic strain brought on by the increased muscle activity. Full recovery takes 4 to 6 weeks because the body must regenerate destroyed nerve axon terminals.
Epidemiology
Tetanus is an international health problem, as C. tetani spores are ubiquitous. The disease occurs almost exclusively in persons who are unvaccinated or inadequately immunized.[1] Tetanus occurs worldwide but is more common in hot, damp climates with soil rich in organic matter. This is particularly true with manure-treated soils, as the spores are widely distributed in the intestines and feces of many non-human animals such as horses, sheep, cattle, dogs, cats, rats, guinea pigs, and chickens. Spores can be introduced into the body through puncture wounds. In agricultural areas, a significant number of human adults may harbor the organism. The spores can also be found on skin surfaces and in contaminated heroin.[2] Heroin users, particularly those that inject the drug, appear to be at high risk for tetanus.
Tetanus – particularly the neonatal form – remains a significant public health problem in non-industrialized countries. There are about one million cases of tetanus reported worldwide annually, causing an estimated 300,000 to 500,000 deaths each year.[2]
In the United States, approximately 100 people become infected with tetanus each year, and there are about five deaths from tetanus each year.[13] Nearly all of the cases in the United States occur in unimmunized individuals or individuals who have allowed their inoculations to lapse,[13] whereas most cases in developing countries are due to the neonatal form of tetanus.
Tetanus is the only vaccine-preventable disease that is infectious but is not contagious.[2][13]
History
Tetanus was well known to ancient people who recognized the relationship between wounds and fatal muscle spasms. The word "tetanus" is derived from the Greek τέτανος tetanos meaning "taut", and τείνειν teinein to "stretch".[14] In 1884, Arthur Nicolaier isolated the strychnine-like toxin of tetanus from free-living, anaerobic soil bacteria. The etiology of the disease was further elucidated in 1884 by Antonio Carle and Giorgio Rattone, who demonstrated the transmissibility of tetanus for the first time. They produced tetanus in rabbits by injecting pus from a patient with fatal tetanus into their sciatic nerves. In 1889, C. tetani was isolated from a human victim by Kitasato Shibasaburo, who later showed that the organism could produce disease when injected into animals, and that the toxin could be neutralized by specific antibodies. In 1897, Edmond Nocard showed that tetanus antitoxin induced passive immunity in humans, and could be used for prophylaxis and treatment. Tetanus toxoid vaccine was developed by P. Descombey in 1924, and was widely used to prevent tetanus induced by battle wounds during World War II.[2]
Notable victims
- Tom Butler – English footballer; contracted after suffering a badly broken arm.
- George Hogg – English adventurer who rescued war orphans in China; died in 1945 from an infection resulting from a foot injury.
- Joe Hill Louis – Memphis blues musician; died in 1957 as a result of an infected wound to his thumb.
- George Montagu – English ornithologist; contracted tetanus when he stepped on a nail.
- Joe Powell – English footballer; contracted following amputation of a badly broken arm.
- John A. Roebling – Civil Engineer and Architect famous for his bridge designs, particularly the Brooklyn Bridge; contracted tetanus following amputation of his foot due to an injury caused by a ferry when it crashed into a wharf.
- George Crockett Strong – Union brigadier general in the American Civil War; from wounds sustained in the assault against Fort Wagner on Morris Island, South Carolina.
- Fred Thomson – silent film actor; stepped on a nail.
- John Thoreau (brother of Henry David Thoreau); nicked himself with a razor while shaving.
- Johann Tserclaes, Count of Tilly; wounded by a cannon ball in the Battle of Rain.
- Traveller – General Robert E. Lee's favorite horse; stepped on a nail.
See also
- Tetanized state
References
- ↑ 1.0 1.1 Wells CL, Wilkins TD (1996). "Clostridia: Sporeforming Anaerobic Bacilli". In Baron S, et alublisher = Univ of Texas Medical Branch. Baron's Medical Microbiology. ISBN 0-9631172-1-1. http://www.ncbi.nlm.nih.gov/books/bv.fcgi?rid=mmed.section.1099.
- ↑ 2.0 2.1 2.2 2.3 2.4 2.5 2.6 2.7 "Tetanus" (PDF). CDC Pink Book. http://www.cdc.gov/vaccines/pubs/pinkbook/downloads/tetanus.pdf. Retrieved 2007-01-26.
- ↑ Vandelaer J; Birmingham M; Gasse F; Kurian M; Shaw C; Garnier S (July 28, 2003). "Tetanus in developing countries: an update on the Maternal and Neonatal Tetanus Elimination Initiative". Vaccine 21 (24): 3442–5. doi:10.1016/S0264-410X(03)00347-5. PMID 12850356.
- ↑ Brauner JS; Vieira SR; Bleck TP (July 2002). "Changes in severe accidental tetanus mortality in the ICU during two decades in Brazil". Intensive Care Medicine 28 (7): 930–5. doi:10.1007/s00134-002-1332-4. PMID 12122532.
- ↑ 5.0 5.1 5.2 5.3 Farrar JJ; Yen LM; Cook T; Fairweather N; Binh N; Parry J; Parry CM (September 2000). "Tetanus". Journal of Neurology, Neurosurgery, and Psychiatry 69 (3): 292–301. PMID 10945801.
- ↑ World Health Organization (2000-11-01). "Maternal and Neonatal Tetanus Elimination by 2005". http://www.unicef.org/immunization/files/MNTE_strategy_paper.pdf#search=%22neonatal%20tetanus%20rates%22. Retrieved 2007-01-26.
- ↑ AU Lalli G; Gschmeissner S; Schiavo G (November 15, 2003). "Myosin Va and microtubule-based motors are required for fast axonal retrograde transport of tetanus toxin in motor neurons". Journal of Cell Science 116 (Pt 22): 4639–50. doi:10.1242/jcs.00727. PMID 14576357.
- ↑ Schiavo G; Benfenati F; Poulain B; Rossetto O; Polverino de Laureto P; DasGupta BR; Montecucco C (October 29, 1992). "Tetanus and botulinum-B neurotoxins block neurotransmitter release by proteolytic cleavage of synaptobrevin". Nature 359 (6398): 832–5. doi:10.1038/359832a0. PMID 1331807.
- ↑ Nitin M. Apte and Dilip R. Karnad (1995-10). "Short Report: The Spatula Test: A Simple Bedside Test to Diagnose Tetanus". Am. J. Trop. Med. Hyg.. pp. 386–387. http://www.ajtmh.org/cgi/content/abstract/53/4/386. Retrieved 2007-10-11.
- ↑ 10.0 10.1 Hopkins, A.; Lahiri, T.; Salerno, R.; Heath, B. (1991). "Diphtheria, tetanus, and pertussis: recommendations for vaccine use and other preventive measures. Recommendations of the Immunization Practices Advisory committee (ACIP).". MMWR Recomm Rep 40 (RR-10): 1–28. doi:10.1542/peds.2006-0692. PMID 1865873.
- ↑ http://www.cdc.gov/vaccines/vpd-vac/tetanus/default.htm#vacc
- ↑ Porter JD, Perkin MA, Corbel MJ, Farrington CP, Watkins JT, Begg NT (1992). "Lack of early antitoxin response to tetanus booster". Vaccine 10 (5): 334–6. doi:10.1016/0264-410X(92)90373-R. PMID 1574917.
- ↑ 13.0 13.1 13.2 Office of Public Information, Missouri Department of Health and Senior Services (2005-07-14). "Tetanus Cases Prompt Advisory for Missourians to Get Vaccine, Check Booster Status". Press release. http://www.dhss.mo.gov/NewsAndPublicNotices/Tetanus7-14-05.html. Retrieved 2006-09-20.
- ↑ Collins English Dictionary – Complete and Unabridged 6th Edition 2003. William Collins Sons & Co. Ltd 1979, 1986 © HarperCollins Publis hers 1991, 1994, 1998, 2000, 2003: via http://www.thefreedictionary.com/tetanus
External links
- Tetanus Information from Medline Plus
- Tetanus Surveillance -- United States, 1998-2000 (Data and Analysis)
Media
|
||||||||||||||||||||||||||||||||||||||||||||||||||||||||