Hysterectomy
| Intervention: Hysterectomy |
||
|---|---|---|
| ICD-10 code: | ||
| ICD-9 code: | 68.9 | |
| MeSH | D007044 | |
| Other codes: | ||
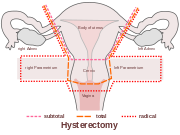
A hysterectomy (from Greek ὑστέρα hystera "womb" and εκτομία ektomia "a cutting out of") is the surgical removal of the uterus, usually performed by a gynecologist. Hysterectomy may be total (removing the body, fundus, and cervix of the uterus; often called "complete") or partial (removal of the uterine body while leaving the cervix intact; also called "supracervical"). It is the most commonly performed gynecological surgical procedure. In 2003, over 600,000 hysterectomies were performed in the United States alone, of which over 90% were performed for benign conditions.[1] Such rates being highest in the industrialized world has led to the major controversy that hysterectomies are being largely performed for unwarranted and unnecessary reasons.[2]
Removal of the uterus renders the patient unable to bear children (as does removal of ovaries and fallopian tubes), and changes her hormonal levels considerably, so the surgery is normally recommended for only a few specific circumstances:
- Certain types of reproductive system cancers (uterine, cervical, ovarian) or tumors
- Severe and intractable endometriosis (growth of the uterine lining outside the uterine cavity) and/or adenomyosis (a form of endometriosis, where the uterine lining has grown into and sometimes through the uterine wall musculature) after pharmaceutical or other surgical options have been exhausted
- Postpartum to remove either a severe case of placenta praevia (a placenta that has either formed over or inside the birth canal) or placenta percreta (a placenta that has grown into and through the wall of the uterus to attach itself to other organs), as well as a last resort in case of excessive postpartum bleeding
- For transmen, as part of their gender transition
- For severe developmental disabilities
Although hysterectomy is frequently performed for fibroids (benign tumor-like growths inside the uterus itself made up of muscle and connective tissue), conservative options in treatment are available by doctors who are trained and skilled at alternatives. It is well documented in medical literature that myomectomy, surgical removal of fibroids with reconstruction of the uterus, has been performed for over a century.
The uterus is a hormone-responsive reproductive sex organ, and the ovaries produce the majority of estrogen and progesterone that is available in genetic females of reproductive age.
Some women's health education groups such as the Hysterectomy Educational Resources and Services (HERS) Foundation seek to inform the public about the many consequences and alternatives to hysterectomy, and the important functions that the female organs have all throughout a woman's life.[3][4][5]
Contents |
Incidence
Canada
In Canada, the number of hysterectomies between 2008 and 2009 was almost 47,000. The national rate in for the same timeline was 338 per 100,000 population, down from 484 per 100,000 in 1997. The reasons for hysterectomies differed depending on whether the woman was living in an urban or rural location. Urban women most common reason was due to uterine fibroids and rural women had hysterectomies mostly for menstrual disorders.[6]
United States
According to the National Center for Health Statistics, of the 617,000 hysterectomies performed in 2004, 73% also involved the surgical removal of the ovaries. In the United States, 1/3 of women can be expected to have a hysterectomy by age 60.[7] There are currently an estimated 22 million people in the United States who have undergone this procedure. An average of 622,000 hysterectomies a year have been performed for the past decade.[7]
United Kingdom
In the UK, one in 5 women is likely to have a hysterectomy by age 60, and ovaries are removed in about 20% of hysterectomies.[8]
Indications
Hysterectomy is usually performed for problems with the uterus itself or problems with the entire female reproductive complex. Some of the conditions treated by hysterectomy include uterine fibroids (myomas), endometriosis (growth of tissue resembling the uterine lining tissue outside of the uterine cavity), adenomyosis (a more severe form of endometriosis, where the uterine lining has grown into and sometimes through the uterine wall), several forms of vaginal prolapse, heavy or abnormal menstrual bleeding, and at least three forms of cancer (uterine, advanced cervical, ovarian). Hysterectomy is also a surgical last resort in uncontrollable postpartum obstetrical haemorrhage.[9]
Uterine fibroids, although a benign disease, may cause heavy menstrual flow and discomfort to some of those with the condition. Many alternative treatments are available: pharmaceutical options (the use of NSAIDs or opiates for the pain and hormones to suppress the menstrual cycle); myomectomy (removal of uterine fibroids while leaving the uterus intact); uterine artery embolization, high intensity focused ultrasound or watchful waiting. In mild cases, no treatment is necessary. If the fibroids are inside the lining of the uterus (submucosal), and are smaller than 4 cm, hysteroscopic removal is an option. A submucosal fibroid larger than 4 cm, and fibroids located in other parts of the uterus, can be removed with a laparotomic myomectomy, where a horizontal incision is made above the pubic bone for better access to the uterus.
Hysterectomy was in the past sometimes performed as a prophylactic treatment for those with either a strong family history of reproductive system cancers (especially breast cancer in conjunction with BRCA1 or BRCA2 mutation) or as part of their recovery from such cancers. With the availability of new medications such as raloxifene, aromatase inhibitors and more recent prophylactic strategies for high risk BRCA mutations this is should be an extremely rare indication for hysterectomy.
Types of hysterectomy
Hysterectomy in the literal sense of the word means merely removal of the uterus, however other organs such as ovaries, fallopian tubes and the cervix are very frequently removed as part of the surgery.
- Radical hysterectomy : complete removal of the uterus, cervix, upper vagina, and parametrium. Indicated for cancer. Lymph nodes, ovaries and fallopian tubes are also usually removed in this situation.
- Total hysterectomy : Complete removal of the uterus and cervix.
- Subtotal hysterectomy : removal of the uterus, leaving the cervix in situ.
Many women want to retain the cervix believing that it may affect sexual satisfaction after hysterectomy. It has been postulated that removing the cervix causes excessive neurologic and anatomic disruption, thus leading to vaginal shortening, vaginal vault prolapse, and vaginal cuff granulations. These issues were addressed in a systematic review of total versus supracervical hysterectomy for benign gynecological conditions, which reported the following findings[10]:
- There was no difference in the rates of incontinence, constipation or measures of sexual function.
- Length of surgery and amount of blood lost during surgery were significantly reduced during supracervical hysterectomy compared to total hysterectomy, but there was no difference in post-operative transfusion rates.
- Febrile morbidity was less likely and ongoing cyclic vaginal bleeding one year after surgery was more likely after supracervical hysterectomy.
- There was no difference in the rates of other complications, recovery from surgery, or readmission rates.
In the short-term, randomized trials have shown that cervical preservation or removal does not affect the rate of subsequent pelvic organ prolapse.[11] However, no trials to date have addressed the risk of pelvic organ prolapse many years after surgery, which may differ after total versus supracervical hysterectomy. It is obvious that supracervical hysterectomy does not eliminate the possibility of having cervical cancer since the cervix itself is left intact. Those who have undergone this procedure must still have regular Pap smears to check for cervical dysplasia or cancer.
Technique
Hysterectomy can be performed in different ways. The oldest known technique is abdominal incision. Subsequently the vaginal (performing the hysterectomy through the vaginal canal) and later laparoscopic vaginal (with additional instruments inserted through a small hole, frequently close to the navel) techniques were developed.
Most hysterectomies in the United States are done via laparotomy (abdominal incision, not to be confused with laparoscopy). A transverse (Pfannenstiel) incision is made through the abdominal wall, usually above the pubic bone, as close to the upper hair line of the individual's lower pelvis as possible, similar to the incision made for a caesarean section. This technique allows doctors the greatest access to the reproductive structures and is normally done for removal of the entire reproductive complex. The recovery time for an open hysterectomy is 4–6 weeks and sometimes longer due to the need to cut through the abdominal wall. Historically, the biggest problem with this technique were infections, but infection rates are well-controlled and not a major concern in modern medical practice. An open hysterectomy provides the most effective way to explore the abdominal cavity and perform complicated surgeries. Before the refinement of the vaginal and laparoscopic vaginal techniques it was also the only possibility to achieve subtotal hysterectomy, meanwhile any of the techniques can be used for subtotal hysterectomy.
Vaginal hysterectomy is performed entirely through the vaginal canal and has clear advantages over abdominal surgery such as less complications, shorter hospital stays and shorter healing time. Abdominal hysterectomy, the most common method, is used in cases such as after caesarean delivery, when the indication is cancer, when complications are expected or surgical exploration is required. The average vaginal-to-abdominal hysterectomy quotient (VAQ) in US residency programs is 0.50.[12]
With the development of the laparoscopic techniques in the 1970-1980s, the "laparoscopic-assisted vaginal hysterectomy" (LAVH) has gained great popularity among gynecologists because compared with the abdominal procedure it is less invasive and the post-operative recovery is much faster. It also allows better exploration and slightly more complicated surgeries then the vaginal procedure. LAVH begins with laparoscopy and is completed such that the final removal of the uterus (with or without removal of the ovaries) is via the vaginal canal. Thus, LAVH is also a total hysterectomy, the cervix must be removed with the uterus. Total laparoscopic hysterectomy (TLH) is more advanced than an LAVH and does not require a double-setup, laparoscopic and vaginal.[13] In OBGYN residency programs, the average laparoscopy-to-laparotomy quotient (LPQ) is 0.55.[12]
The "laparoscopic-assisted supracervical hysterectomy" (LASH) was later developed to remove the uterus without removing the cervix using a morcellator which cuts the uterus into small pieces that can be removed from the abdominal cavity via the laparoscopic ports.
Total laparoscopic hysterectomy (TLH) is performed solely through the laparoscopes in the abdomen, starting at the top of the uterus. The entire uterus is disconnected from its attachments using long thin instruments through the "ports". Then all tissue to be removed is passed through the small abdominal incisions.
Supracervical (subtotal) laparoscopic hysterectomy (LSH) is performed similar to the total laparoscopic surgery but the uterus is amputated between the cervix and fundus.
"Robotic hysterectomy" is a variant of laparoscopic surgery using special remotely controlled instruments that allow the surgeon finer control as well as three-dimensional magnified vision.[14]
 uterus before hysterectomy |
 laparoscopical hysterectomy |
 transvaginal extraction of the uterus in total laparoscopical hysterectomy |
 cervical stump (white) after removement of the uterine corpus at laparoscopic supracervical hysterectomy |
 end of an laparoscopical hysterectomy |
Comparison of techniques
The abdominal technique is very often applied in difficult circumstances or when complications are expected. Given this circumstances the complication rate and time required for surgery compares very favorably with other techniques, however time required for healing is much longer.
Vaginal hysterectomy was shown to be superior to LAVH and some types of laparoscopic surgery (sufficient data was not available for all types of laparoscopic surgery), causing fewer short- and long-term complications, more favorable effect on sexual experience with shorter recovery times and fewer costs.[15][16][17] It is however not possible or very difficult to perform some more complicated surgeries using this technique.
A recent Cochrane review recommends vaginal hysterectomy over other variants where possible. Laparoscopic surgery offers certain advantages when vaginal surgery is not possible but has also the disadvantage of significantly longer time required for the surgery.[18]
In direct comparison of abdominal (laparotomic) and laparoscopic techniques laparoscopic surgery causes longer operation time and substantially higher rate of major complications while offering much quicker healing.[18][19]
Vaginal hysterectomy is the only available option that is feasible without total anaesthesia or in outpatient settings (although so far recommended only in exceptional cases).
Time required for completion of surgery in the eVAL trial is reported as following:[19]
- abdominal 55.2 minutes average, range 19-155
- vaginal 46.6 minutes average, range 14-168
- laproscopic (all variants) 82.5 minutes average, range 10-325 (combined data from both trial arms)
Large multifibroid uteri and subtotal hysterectomies did previously require abdominal incision but with the use of in situ morcellation they can be sometimes also performed using laparoscopic or vaginal techniques.[20] Even impacted fibroid uteri with severe adhesions, oblitered cul-de-sac and no motion whatsoever on pelvic exam can be removed laparoscopically by experienced laparoscopic surgeons.[21] An advanced laparoscopist can replace the majority of inpatient total abdominal hysterectomies performed for benign indications with outpatient total laparoscopic hysterectomy.[22]
Non-robotic laparoscopic hysterectomy has a higher likelihood a requiring a large incision and conversion to open technique than robotic hysterectomy. In addition blood loss and duration of hospital stay were lower when using robotic technique when compared to non-robotic laparoscopic hysterectomy.[23]
The other techniques are not long enough in use to allow a general assessment, it appears that laparoscopic subtotal hysterectomy(LSH) is a promising technique.[16]
Benefits
Hysterectomy is usually performed for serious conditions and is highly effective in curing those conditions.
The Maine Women's Health Study of 1994 followed for 12 months time approximately 800 women with similar gynecological problems (pelvic pain, urinary incontinence due to uterine prolapse, severe endometriosis, excessive menstrual bleeding, large fibroids, painful intercourse), around half of whom had a hysterectomy and half of whom did not. The study found that a substantial number of those who had a hysterectomy had marked improvement in their symptoms following hysterectomy, as well as significant improvement in their overall physical and mental health one year out from their surgery. The study concluded that for those who have intractable gynecological problems that had not responded to non-surgical intervention, hysterectomy may be beneficial to their overall health and wellness. Somewhat surprisingly, ovarian cancer risk after hysterectomy appears to be substantially lowered even when the ovaries are preserved.[24]
Risks and side effects
Hysterectomy has like any other surgery certain risks and side effects.
Mortality and surgical risks
Short term mortality (within 40 days of surgery) is usually reported in the range of 1-6 cases per 1000 when performed for benign causes.[25] The mortality rate is several times higher when performed in patients that are pregnant, have cancer or other complications.[26]
Long term effect on all case mortality is relatively small. Women under the age of 45 years have a significantly increased long term mortality that is believed to be caused by the hormonal side effects of hysterectomy and prophylactic oophorectomy.[27]
Approximately 35% of women after hysterectomy undergo another related surgery within 2 years.
Reconvalescence
Hospital stay is 3 to 5 days or more for the abdominal procedure and between 2 to 3 days for vaginal or laparoscopically assisted vaginal procedures.
Time for full recovery is very long and practically independent on the procedure that was used. Depending on the definition of "full recovery" 6 to 12 months have been reported. Serious limitations in everyday activities are expected for a minimum of 4 months.
Unintended oophorectomy and premature ovarian failure
Removal of one or both ovaries is performed in a substantial number of hysterectomies that were intended to be ovariesparing.[28]
The average onset age of menopause in those who underwent hysterectomy is 3.7 years earlier than average even when the ovaries are preserved.[29] This has been suggested to be due to the disruption of blood supply to the ovaries after a hysterectomy or due to missing endocrine feedback of the uterus. The function of the remaining ovaries is significantly affected in about 40% women, some of them even require hormone replacement treatment. Surprisingly, a similar and only slightly weaker effect has been also observed for endometrial ablation which is often considered as an alternative to hysterectomy.
Substantial number of women develop benign ovarian cysts after hysterectomy.[30]
Premature menopause and its effects
Estrogen levels fall sharply when the ovaries are removed, removing the protective effects of estrogen on the cardiovascular and skeletal systems. This condition is often referred to as "surgical menopause", although it is substantially different from a naturally occurring menopausal state; the former is a sudden hormonal shock to the body that causes rapid onset of menopausal symptoms such as hot flashes, while the latter is a gradually occurring decrease of hormonal levels over a period of years with uterus intact and ovaries able to produce hormones even after the cessation of menstrual periods.
When only the uterus is removed there is a three times greater risk of cardiovascular disease. If the ovaries are removed the risk is seven times greater. Several studies have found that osteoporosis (decrease in bone density) and increased risk of bone fractures are associated with hysterectomies.[31][32][33][34][35][36] This has been attributed to the modulatory effect of estrogen on calcium metabolism and the drop in serum estrogen levels after menopause can cause excessive loss of calcium leading to bone wasting.
Hysterectomies have also been linked with higher rates of heart disease and weakened bones. Those who have undergone a hysterectomy with both ovaries removed typically have reduced testosterone levels as compared to those left intact.[28] Reduced levels of testosterone in women is predictive of height loss, which may occur as a result of reduced bone density,[37] while increased testosterone levels in women are associated with a greater sense of sexual desire.[38]
Oophorectomy before the age of 45 is associated with a fivefold mortality from neurologic and mental disorders.[39]
Urinary incontinence and vaginal prolapse
Urinary incontinence and vaginal prolapse are well known adverse effects that develop with high frequency very long time after the surgery. Typically those complications develop 10–20 years after the surgery.[40] For this reason exact numbers are not known and risk factors poorly understood, it is also unknown if the choice surgical technique has any effect. It has been assessed that the risk for urinary incontinence is approximately doubled within 20 years after hysterectomy. One long term study found a 2.4 fold increased risk for surgery to correct urinary stress incontinence following hysterectomy [41][42]
The risk for vaginal prolapse is over 80% within 20 years of hysterectomy.
Effects on social life and sexuality
Some women find their natural lubrication during sexual arousal is also reduced or eliminated. Those who experience uterine orgasm will not experience it if the uterus is removed. The vagina is shortened and made into a closed pocket and there is a loss of support to the bladder and bowel.
Other rare problems
Hysterectomy may cause an increased risk of the relatively rare renal cell carcinoma. Hormonal effects or injury of the ureter were considered as possible explanations.[43][44]
Removal of the uterus without removing the ovaries can produce a situation that on rare occasions can result in ectopic pregnancy due to an undetected fertilization that had yet to descend into the uterus before surgery. Two cases have been identified and profiled in an issue of the Blackwell Journal of Obstetrics and Gynecology; over 20 other cases have been discussed in additional medical literature.[45]
Alternatives


Depending on the problem there are alternatives to hysterectomy :
Heavy bleeding
Dysfunctional uterine bleeding (DUB) may be treated with endometrial ablation, which is an outpatient procedure in which the lining of the uterus is destroyed with heat, mechanically or by radio frequency ablation. Endometrial ablation will greatly reduce or entirely eliminate monthly bleeding in ninety percent of patients with DUB. It is not effective for patients with very thick uterine lining or uterine fibroids.
Menorrhagia (heavy or abnormal menstrual bleeding) may also be treated with the less invasive endometrial ablation.[46]
See also Mirena coil which releases low dose progesterone.
Uterine fibroids
Uterine fibroids may be removed and the uterus reconstructed in a procedure called "myomectomy." A myomectomy may be performed through an open incision, laparoscopically or through the vagina (hysterescopy).[47]
Uterine artery embolization is a minimally invasive procedure for treatment of uterine fibroids. Under local anesthesia a catheter is introduced into the femoral artery at the groin and advanced under radiographic control into the uterine arterty. A mass of microspheres or polyvinyl alcohol (PVA) material (an embolus) is injected into the uterine arteries in order to block the flow of blood through those vessels. The restriction in blood supply usually results in in significant reduction of fibroids and improvement of heavy bleeding tendency. The 2006 Cochrane review comparing hysterectomy and UAE did not find any major advantage for either procedure.[48] The subsequently finished HOPEFUL study found substantially fewer serious adverse effects for UAE with lesser overall cost and comparable satisfaction. In this study 86% UAE treated women and 70% hysterectomy treated women recommend their treatment to a friend. [49]
Uterine fibroids can be treated also with a non-invasive procedure called Magnetic Resonance guided Focused Ultrasound (MRgFUS). This procedure involves no cutting or general anesthesia and the uterus remains intact.
Prolapse
Prolapse may also be corrected surgically without removal of the uterus. [50]
As part of transitioning from female-to-male
Hysterectomies with bilateral salpingo-oophorectomy are often performed either prior to or as a part of sex reassignment surgery for transmen. Some in the FTM community prefer to have this operation along with hormone replacement therapy in the early stages of their gender transition to avoid complications from heavy testosterone use while still having female-hormone-producing organs in place (e.g. uterine cancer and hormonally induced coronary artery disease) or to remove as many sources of female sex hormones as possible in order to better "pass" during the real life experience portion of their transition.[51] Just as many, however, prefer to wait until they have full "bottom surgery" (removal of female sexual organs and construction of male-appearing external anatomy)[52] to avoid undergoing multiple separate operations.[53]
See also
- Hysterectomy Educational Resources and Services (HERS) Foundation
- Michael Neary
References
- ↑ Wu, JM, Wechter, ME, Geller, EJ, et al. Hysterectomy rates in the United States, 2003. Obstet Gynecol 2007; 110:1091
- ↑ "Are Hysterectomies Too Common?". TIME Magazine. 2006-07-01. http://www.time.com/time/health/article/0,8599,1644050,00.html?cnn=yes. Retrieved 2007-07-17.
- ↑ "Facts about hysterectomy". Hysterectomy Alternatives and Aftereffects. http://www.hersfoundation.org/facts.html. Retrieved 2007-06-07.
- ↑ "Female Anatomy: the Functions of Female Organs". Hysterectomy Alternatives and Aftereffects. http://hersfoundation.org/anatomy/index.html. Retrieved 2007-06-07.
- ↑ "Hysterectomy Educational Resources & Services". Hysterectomy Alternatives and Consequences. http://hersfoundation.org/. Retrieved 2009-02-13.
- ↑ "Hysterectomy rates falling: report". CBC News. 2010-05-27. http://www.cbc.ca/health/story/2010/05/27/hysterectomy-canada.html. Retrieved 2010-05-28.
- ↑ 7.0 7.1 "Hysterectomy". National Women’s Health Information Center. 2006-07-01. http://www.4women.gov/faq/hysterectomy.htm. Retrieved 2007-06-07.
- ↑ Gautam Khastgir, John Studd (1998). Hysterectomy and HRT. Taylor & Francis. p. 3. ISBN 9781853174087. http://books.google.com/?id=v-ENVtKsRhUC&pg=PA1&lpg=PA1&dq=hysterectomy+incidence.
- ↑ Roopnarinesingh R, Fay L, McKenna P (2003). "A 27-year review of obstetric hysterectomy". Journal of obstetrics and gynaecology : the journal of the Institute of Obstetrics and Gynaecology 23 (3): 252–4. PMID 12850853.
- ↑ Lethaby, A, Ivanova, V, Johnson, NP. Total versus subtotal hysterectomy for benign gynecological conditions. Cochrane Database Syst Rev 2006; CD004993
- ↑ Thakar, R, Ayers, S, Clarkson, P, Stanton, S, et aI. Outcomes after Total versus Subtotal abdominal hysterectomy. N Engl J Med 2002; 347;1318
- ↑ 12.0 12.1 Walid MS, Heaton RL (2010). "Laparoscopy-to-laparotomy quotient in obstetrics and gynecology residency programs". Arch Gyn Ob. doi:10.1007/s00404-010-1477-2. PMID 20414665.
- ↑ Walid MS, Heaton RL (2010). "Total laparoscopic hysterectomy in 26 min.". Arch Gyn Ob 281 (6): 1077–8. doi:10.1007/s00404-009-1312-9. PMID 20012980.
- ↑ Medline Plus: Robotic surgery
- ↑ PMID 8672159 (PubMed)
Citation will be completed automatically in a few minutes. Jump the queue or expand by hand - ↑ 16.0 16.1 "Laparoscopic Hysterectomy and Health Care in America - Finding the Balance Between Costs and Outcomes". http://www.obgyn.net/hysterectomy-alternatives/hysterectomy-alternatives.asp?page=articles/daniell_hysttrends. Retrieved 2010-01-24.
- ↑ Debodinance, P (2001). "Hysterectomy for benign lesions in the north of France: epidemiology and postoperative events". Journal de gynecologie, obstetrique et biologie de la reproduction 30 (2): 151–9. PMID 11319467.
- ↑ 18.0 18.1 PMID 19588344 (PubMed)
Citation will be completed automatically in a few minutes. Jump the queue or expand by hand - ↑ 19.0 19.1 PMID 14711749 (PubMed)
Citation will be completed automatically in a few minutes. Jump the queue or expand by hand - ↑ Walid MS, Heaton RL. (2009). "Laparoscopic extirpation of a 3-kg uterus". Arch Gynecol Obstet. 279 (4): 607–608. doi:10.1007/s00404-008-0827-9. ISSN 0932-0067. PMID 19011884.
- ↑ Walid MS, Heaton RL. (2010). "Total laparoscopic extirpation of a fixed uterus from benign gynecological disease". Gynecological Surgery. doi:10.1007/s10397-010-0558-3. ISSN 1613-2084.
- ↑ Heaton RL, Walid MS. (2010). "An intention-to-treat study of total laparoscopic hysterectomy". Int J Gynaecol Obstet. doi:10.1016/j.ijgo.2010.04.027. ISSN 1879-3479. PMID 20557885.
- ↑ PMID 18439499 (PubMed)
Citation will be completed automatically in a few minutes. Jump the queue or expand by hand - ↑ Parker WH. "Hysterectomy--A Gynecologist's Second Opinion". http://www.gynsecondopinion.com/hysterectomy.htm. Retrieved 2007-06-07.
- ↑ PMID 15198759 (PubMed)
Citation will be completed automatically in a few minutes. Jump the queue or expand by hand - ↑ PMID 4025434 (PubMed)
Citation will be completed automatically in a few minutes. Jump the queue or expand by hand - ↑ PMID 18714076 (PubMed)
Citation will be completed automatically in a few minutes. Jump the queue or expand by hand - ↑ 28.0 28.1 Laughlin GA, Barrett-Connor E, Kritz-Silverstein D, von Mühlen D (2000). "Hysterectomy, oophorectomy, and endogenous sex hormone levels in older women: the Rancho Bernardo Study". J. Clin. Endocrinol. Metab. 85 (2): 645–51. doi:10.1210/jc.85.2.645. PMID 10690870.
- ↑ Farquhar CM, Sadler L, Harvey SA, Stewart AW (2005). "The association of hysterectomy and menopause: a prospective cohort study". BJOG : an international journal of obstetrics and gynaecology 112 (7): 956–62. doi:10.1111/j.1471-0528.2005.00696.x. PMID 15957999.
- ↑ PMID 15661947 (PubMed)
Citation will be completed automatically in a few minutes. Jump the queue or expand by hand - ↑ Kelsey JL, Prill MM, Keegan TH, Quesenberry CP, Sidney S (2005). "Risk factors for pelvis fracture in older persons". Am. J. Epidemiol. 162 (9): 879–86. doi:10.1093/aje/kwi295. PMID 16221810.
- ↑ van der Voort DJ, Geusens PP, Dinant GJ (2001). "Risk factors for osteoporosis related to their outcome: fractures". Osteoporosis international : a journal established as result of cooperation between the European Foundation for Osteoporosis and the National Osteoporosis Foundation of the USA 12 (8): 630–8. PMID 11580076.
- ↑ Watson NR, Studd JW, Garnett T, Savvas M, Milligan P (1995). "Bone loss after hysterectomy with ovarian conservation". Obstetrics and gynecology 86 (1): 72–7. doi:10.1016/0029-7844(95)00100-6. PMID 7784026.
- ↑ Durães Simões R, Chada Baracat E, Szjenfeld VL, de Lima GR, José Gonçalves W, de Carvalho Ramos Bortoletto C (1995). "Effects of simple hysterectomy on bone loss". São Paulo medical journal = Revista paulista de medicina 113 (6): 1012–5. PMID 8731286.
- ↑ Hreshchyshyn MM, Hopkins A, Zylstra S, Anbar M (1988). "Effects of natural menopause, hysterectomy, and oophorectomy on lumbar spine and femoral neck bone densities". Obstetrics and gynecology 72 (4): 631–8. PMID 3419740.
- ↑ Menon RK, Okonofua FE, Agnew JE, et al. (1987). "Endocrine and metabolic effects of simple hysterectomy". International journal of gynaecology and obstetrics: the official organ of the International Federation of Gynaecology and Obstetrics 25 (6): 459–63. PMID 2892704.
- ↑ Jassal SK, Barrett-Connor E, Edelstein SL (1995). "Low bioavailable testosterone levels predict future height loss in postmenopausal women". J. Bone Miner. Res. 10 (4): 650–4. doi:10.1002/jbmr.5650100419. PMID 7610937.
- ↑ Segraves R, Woodard T (2006). "Female hypoactive sexual desire disorder: History and current status". The journal of sexual medicine 3 (3): 408–18. doi:10.1111/j.1743-6109.2006.00246.x. PMID 16681466.
- ↑ PMID 19365140 (PubMed)
Citation will be completed automatically in a few minutes. Jump the queue or expand by hand - ↑ PMID 10950229 (PubMed)
Citation will be completed automatically in a few minutes. Jump the queue or expand by hand - ↑ PMID 17964350 (PubMed)
Citation will be completed automatically in a few minutes. Jump the queue or expand by hand - ↑ McPherson K, Herbert A, Judge A, et al. (2005). "Self-reported bladder function five years post-hysterectomy". Journal of obstetrics and gynaecology : the journal of the Institute of Obstetrics and Gynaecology 25 (5): 469–75. doi:10.1080/01443610500235170. PMID 16183583.
- ↑ PMID 10566555 (PubMed)
Citation will be completed automatically in a few minutes. Jump the queue or expand by hand - ↑ PMID 18711701 (PubMed)
Citation will be completed automatically in a few minutes. Jump the queue or expand by hand - ↑ "Early Ectopic Pregnancy after Vaginal Hysterectomy", P.S. Cocks, published August 23, 2005; retrieved September 7, 2007.
- ↑ Health.com: 5 operations you don't want to get - and what to do instead
- ↑ William H. Parker, Rachel L. Parker, "A Gynecologist's Second Opinion: The Questions & Answers You Need to Take Charge of Your Health," 2002, Plume; Rev ed., 89-92, 105-150.
- ↑ PMID 16437515 (PubMed)
Citation will be completed automatically in a few minutes. Jump the queue or expand by hand - ↑ PMID 18331704 (PubMed)
Citation will be completed automatically in a few minutes. Jump the queue or expand by hand - ↑ Frederick R. Jelovsek, "Having Prolapse, Cystocele and Rectocele Fixed Without Hysterectomy"
- ↑ Hudson's FTM Resource Guide, "Why Have A Hysterectomy?", retrieved May 8, 2007.
- ↑ Hudson's FTM Resource Guide, "FTM Gender Reassignment Surgery, retrieved May 9, 2007.
- ↑ Hudson's FTM Resource Guide, "Types of Hysterectomy", retrieved May 8, 2007.
External links
- laparoscopic hysterectomy
- Female Anatomy: Functions of the Female Organs
- Hysterectomy at the Open Directory Project
- Hysterectomy at the Open Directory Project (Hysterectomy Support Groups)
- Medline article on Hysterectomy
|
||||||||||||||||||||||||||||