Paroxetine
 |
|
|---|---|
 |
|
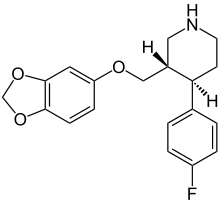
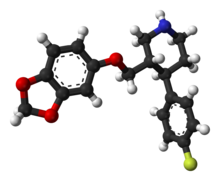
| Systematic (IUPAC) name | |
| (3S,4R)-3-[(2H-1,3-benzodioxol-5-yloxy)methyl]-4-(4-fluorophenyl)piperidine | |
| Identifiers | |
| CAS number | 61869-08-7 |
| ATC code | N06AB05 |
| PubChem | CID 43815 |
| DrugBank | DB00715 |
| ChemSpider | 39888 |
| Chemical data | |
| Formula | C19H20FNO3 |
| Mol. mass | 329.3 |
| SMILES | eMolecules & PubChem |
| Pharmacokinetic data | |
| Bioavailability | Completely absorbed from GI, but extensive first-pass metabolism in the liver; Tmax 4.9 (with meals) to 6.4 hours (fasting) |
| Protein binding | 93–95% |
| Metabolism | Extensive, hepatic (mostly CYP2D6-mediated) |
| Half-life | 24 hours (range 3–65 hours) |
| Excretion | 64% in urine, 36% in bile |
| Therapeutic considerations | |
| Licence data | US FDA:link |
| Pregnancy cat. | D(US) |
| Legal status | ℞ Prescription only |
| Routes | Oral |
| |
|
Paroxetine (trade names Aropax, Paxil) is a selective serotonin reuptake inhibitor (SSRI) antidepressant. Marketing of the drug began in 1992 by the pharmaceutical company SmithKline Beecham, now GlaxoSmithKline. Paroxetine is used to treat major depression, obsessive-compulsive, panic, social anxiety, and generalised anxiety[1] disorders in adult outpatients.
In adults, the efficacy of paroxetine for depression is comparable to that of older tricyclic antidepressants, with fewer side effects and lower toxicity.[2][3] Differences with newer antidepressants are subtler and mostly confined to side effects. It shares the common side effects and contraindications of other SSRIs, with high rates of nausea, somnolence, and sexual side effects. Unlike two other popular SSRI antidepressants, fluoxetine and sertraline, paroxetine is associated with clinically significant weight gain[4] and statistically significant increase in the risk of suicidality in adults.[5] Pediatric trials of paroxetine for depression did not demonstrate efficacy and showed an increase in the risk of harmful outcomes, including episodes of self-harm and potentially suicidal behavior.[6][7][8]
Discontinuing paroxetine is associated with a high risk of discontinuation or withdrawal syndrome.[9][10] Due to the increased risk of birth defects, pregnant women or women planning to become pregnant are recommended to avoid or discontinue paroxetine use.[11][12][13]
Contents |
Indications
Paroxetine is primarily used to treat the symptoms of major depression, obsessive-compulsive disorder (OCD), post-traumatic stress disorder (PTSD), panic disorder, generalized anxiety disorder (GAD),[14] social phobia/social anxiety disorder,[15] and premenstrual dysphoric disorder (PMDD).[16]
Paroxetine was the first antidepressant formally approved in the United States for the treatment of panic attacks.[17]
According to the prescribing information provided by the manufacturer of the Paxil brand of paroxetine (GlaxoSmithKline) and approved by the U.S. Food and Drug Administration (FDA),[18] the effectiveness of paroxetine in major depressive disorder has been proven by six placebo-controlled clinical trials. For panic disorder, three 10-12-week studies indicated paroxetine superiority to placebo.[18] Similarly, three 12-week trials for adult outpatients with social anxiety disorder demonstrated better response to paroxetine than to placebo.[18] Additional studies show patients are 10-20% more likely to benefit compared to placebo.[19]
Unapproved/off-label/investigational
Several studies have suggested that paroxetine can be used in the treatment of premature ejaculation. In particular, intravaginal ejaculation latency time (IELT) was found to increase with 6-13-fold, which was somewhat longer than the delay achieved by the treatment with other SSRIs (fluvoxamine, fluoxetine, sertraline, and citalopram).[20][21][22] However, paroxetine taken acutely ("on demand") 3–10 hours before coitus resulted only in a "clinically irrelevant and sexually unsatisfactory" 1.5-fold delay of ejaculation and was inferior to clomipramine, which induced a fourfold delay.[22]
SSRIs are also highly effective in the treatment of severe premenstrual syndrome[23]; however, paroxetine is contraindicated in women who may become pregnant due to its teratogenicity and its high risk of withdrawal syndrome in both adults and neonates. See Paroxetine and pregnancy.
There is also evidence that paroxetine may be effective in the treatment of compulsive gambling[24] and hot flashes.[25]
Benefits of paroxetine prescription for diabetic neuropathy[26] or chronic tension headache.[27] are uncertain.
Emerging evidence shows that antipsychotics can be used as a supplement or alternative to paroxetine in patients with generalised anxiety disorder.[1]
Although the evidence is conflicting, paroxetine may be effective for the treatment of dysthymia, a chronic disorder which involves depressive symptoms for most days of the year.[28]
Contraindications
Paroxetine is contraindicated in all patients under 18, in all patients taking any of the drugs listed in the interactions section below, and in adult women who are or may become pregnant. Paroxetine may also be contraindicated in many adult men due to sexual and reproductive side effects described below. In the United States, the Food and Drug Administration requires this drug to carry a black box warning, its "most serious type of warning in prescription drug labeling,"[29] due to increased risk of suicidal ideation and behavior. The warning also applies to other SSRIs, but the concern began with reports of suicidal behavior in paroxetine trials, as well as recommendations from the United Kingdom Medicines and Healthcare products Regulatory Agency urging that paroxetine not be used in individuals younger than 18 years.[30]
Side effects
Among the common adverse effects associated with paroxetine treatment of depression and listed in the prescribing information, those with the greatest difference from placebo are nausea (26% on paroxetine vs 9% on placebo), somnolence (23% vs. 9% on placebo), ejaculatory disturbance (13% vs. 0% on placebo), other male genital disorders (10% vs. 0% on placebo), asthenia (15% vs. 6% on placebo), sweating (11% vs. 2% on placebo), dizziness (13% vs. 6% on placebo), insomnia (13% vs. 6% on placebo), dry mouth (18% vs. 12% on placebo), constipation (14% vs. 9% on placebo), and tremor (8% vs. 2% on placebo).[18] Other side effects include headache, agitation, weight gain, impaired memory and paresthesia.[31]
General side effects are mostly present during the first 1–4 weeks while the body acquires a tolerance to the drug, although once this happens, withdrawal can cause a rebound effect with symptoms re-emerging in an exaggerated form for very long periods of time. Almost all SSRIs are known to cause either one or more of these symptoms. A person receiving paroxetine treatment may experience a few, all, or none of the listed side-effects, and most side-effects will disappear or lessen with continued treatment, though some may last throughout the duration. Side effects are also often dose-dependent, with fewer and/or less severe symptoms being reported at lower dosages, and/or more severe symptoms being reported at higher dosages. Increases or changes in dosage may also cause symptoms to reappear or worsen.[18]
On 9 December 2004, the European Medicines Agency's (EMEA) Committee for Medicinal Products for Human Use (CHMP) informed patients, prescribers, and parents that paroxetine should not be prescribed to children. CHMP also gave a warning to prescribers recommending close monitoring of adult patients at high risk of suicidal behaviour and/or suicidal thoughts. CHMP does not prohibit use of paroxetine with high risk adults but urges extreme caution. Due to reports of adverse withdrawal reactions upon terminating treatment, CHMP recommends to reduce gradually over several weeks or months if the decision to withdraw is made.[32] See also Discontinuation syndrome (withdrawal).
The FDA conducted a statistical analysis of paroxetine clinical trials in children and adolescents in 2004, finding a statistically significant 2.7-fold raise in suicide behavior and ideation as compared to placebo; the trend for increased suicidality was observed in both trials for depression and for anxiety disorders.[6] A University of North Carolina review of SSRIs found the average risk of suicide among adolescents was 4%, versus 2% on placebo, and among all patients "the greatest risk of self-harm was among paroxetine users."[33]
Cases of akathisia[34][35] and activation syndrome[36][37] have been observed during paroxetine treatment.
Rarely serotonin syndrome, a severe adverse effect may occur.[38][39]
Paroxetine and other SSRIs have been shown to cause sexual side effects in most patients, both males and females.[40] In males, paroxetine is also linked to sperm DNA fragmentation.[41]
Mania or hypomania may occur as a serious side effect of paroxetine,[42][43][44] affecting up to 8% of psychiatric patients treated. This side effect can occur in individuals with no history of mania but it is more likely to occur in those with bipolar or with a family history of mania.[45]
Schmitt et al. (2001) suggested that paroxetine negatively affects memory (i.e., IQ). In their study, healthy participants given paroxetine for 14 days (20 mg for days 1–7 and 40 mg days 8–14) showed poorer recall of words on day 14 compared to those receiving a placebo.[46] Schmitt et al. did not take into account a significant difference in verbal recall at baseline between the paroxetine and placebo groups, however, and this difference may have been the source of the significant group difference on day 14. Moreover, participants receiving paroxetine recalled as many words at baseline as they recalled on day 14, which is not consistent with the conclusion that paroxetine negatively affects verbal recall.
Discontinuation syndrome (withdrawal)
Many psychoactive medications can cause withdrawal symptoms upon discontinuation from administration. Evidence has shown that paroxetine has among the highest incidence rates and severity of withdrawal syndrome of any medication of its class.[10][47] Common withdrawal symptoms for paroxetine include nausea, dizziness, lightheadedness and vertigo; insomnia, nightmares and vivid dreams; feelings of electricity in the body, as well as crying and anxiety.[48][49] Liquid formulation of paroxetine is available and allows a very gradual decrease of the dose, which may prevent discontinuation syndrome. Another recommendation is to temporarily switch to fluoxetine, which has a longer half-life and thus decreases the severity of discontinuation syndrome.[9][50][51]
In addition, The Lancet published an analysis of World Health Organization data showing SSRIs taken during pregnancy may cause withdrawal symptoms, including convulsions, in newborn children: among "93 suspected cases of SSRI-induced neonatal withdrawal syndrome...64 were associated with paroxetine, 14 with fluoxetine, nine with sertraline, and seven with citalopram."[52]
Paroxetine and pregnancy
The American College of Obstetricians and Gynecologists recommends that pregnant women and women planning to become pregnant should avoid using paroxetine.[11] According to the prescribing information[18] "epidemiological studies have shown that infants born to women who had first trimester paroxetine exposure had an increased risk of cardiovascular malformations, primarily ventricular and atrial septal defects (VSDs and ASDs). In general, septal defects range from those that are symptomatic and may require surgery to those that are asymptomatic and may resolve spontaneously. If a patient becomes pregnant while taking paroxetine, she should be advised of the potential harm to the fetus. Unless the benefits of paroxetine to the mother justify continuing treatment, consideration should be given to either discontinuing paroxetine therapy or switching to another antidepressant. For women who intend to become pregnant or are in their first trimester of pregnancy, paroxetine should only be initiated after consideration of the other available treatment options." These conclusions are supported by multiple systematic reviews and meta-analyses that found that, on average, the use of paroxetine during pregnancy is associated with about 1.5-1.7-fold increase in congenital birth defects, in particular, heart defects.[53][54][55][56][57] A recent non-systematic review in the Journal of Clinical Psychiatry, with the lead author, Salvatore Gentile, reporting to have received material or financial support from GSK, came to a different conclusion: "the teratogenic potential of paroxetine that has been reported in some studies remains unproven." Gentile called for large, epidemiologic, prospective, controlled studies on "mothers who accept taking paroxetine during pregnancy".[58] Other reviews vary on whether the teratogenic risks outweigh the risk of disease relapse if the drug is discontinued: some advocate discontinuation,[53] while others suggest caution;[55] even where the overview of antidepressants generally is favorable, paroxetine is singled out for specific risks.[56] Paroxetine use during pregnancy increases the risk of spontaneous abortion.[59][60]
Abrupt discontinuation of psychotropic drugs during pregnancy can also lead to serious adverse effects.[61]
Counseling is effective in reassuring women to adhere to therapy,[61] but neonatal paroxetine withdrawal symptoms described above have been documented from mothers taking Paxil during pregnancy.[62]
Paroxetine interactions with other drugs
GlaxoSmithKline cautions that drug interactions may create or increase specific risks, including Serotonin Syndrome or Neuroleptic Malignant Syndrome (NMS)-like Reactions:
- The development of a potentially life-threatening serotonin syndrome or Neuroleptic Malignant Syndrome (NMS)-like reactions have been reported with SNRIs and SSRIs alone, including treatment with PAXIL, but particularly with concomitant use of serotonergic drugs (including triptans) with drugs which impair metabolism of serotonin (including MAOIs), or with antipsychotics or other dopamine antagonists.
The prescribing information states that paroxetine should "not be used in combination with an MAOI (including linezolid, an antibiotic which is a reversible non-selective MAOI), or within 14 days of discontinuing treatment with an MAOI," and should not be used in combination with pimozide, thioridazine, tryptophan, or warfarin.[63]
Paroxetine is metabolized by cytochrome P450 2D6. The breast cancer treatment drug tamoxifen is also metabolized to its active state by the same cytochrome. Patients treated with both paroxetine and tamoxifen have an increased risk of death from breast cancer from 24% to 91%, depending on duration of coexposure. [64]
Pharmacology
Paroxetine is the most potent and one of the most specific selective serotonin (5-hydroxytryptamine, 5-HT) reuptake inhibitors (SSRI).[65] This activity of the drug on brain neurons is thought to be responsible for its antidepressant effects.
Paroxetine is a phenylpiperidine derivative which is chemically unrelated to the tricyclic or tetracyclic antidepressants. In receptor binding studies, paroxetine did not exhibit significant affinity for the adrenergic (α1, α2, β), dopaminergic, serotonergic (5HT1, 5HT2), or histamine receptors of rat brain membrane.[reference needed] A weak affinity for the muscarinic acetylcholine and noradrenaline receptors was evident.[reference needed] The predominant metabolites of paroxetine are essentially inactive as 5-HT reuptake inhibitors.[reference needed]
Formulations
Paroxetine CR (controlled release) was shown to be associated with a lower rate of nausea during the first week of treatment than paroxetine immediate release. However, the rate of treatment discontinuation due to nausea was not significantly different.[66]
Overdosage
Acute overdosage is often manifested by emesis, lethargy, ataxia, tachycardia and seizures. Plasma, serum or blood concentrations of paroxetine may be measured to monitor therapeutic administration, confirm a diagnosis of poisoning in hospitalized patients or to aid in the medicolegal investigation of fatalities. Plasma paroxetine concentrations are generally in a range of 40-400 μg/L in persons receiving daily therapeutic doses and 200-2000 μg/L in poisoned patients. Postmortem blood levels have ranged from 1-4 mg/L in acute lethal overdose situations.[67][68]
Controversy
For 10 years, GlaxoSmithKline (GSK) marketing of the drug stated that it was "not habit forming," which numerous experts and at least one court found to be incorrect.[47][69][70][71] In 2001, the BBC reported the World Health Organization had ranked paroxetine as the most difficult antidepressant to withdraw from.[72] In 2002, the U.S. FDA published a new product warning about the drug, and the International Federation of Pharmaceutical Manufacturers Associations said GSK had misled the public about paroxetine and breached two of the Federation's codes of practice.[10][73] The British Medical Journal quoted Charles Medawar, head of Social Audit: "This drug has been promoted for years as safe and easy to discontinue.... The fact that it can cause intolerable withdrawal symptoms of the kind that could lead to dependence is enormously important to patients, doctors, investors, and the company. GlaxoSmithKline has evaded the issue since it was granted a license for paroxetine over 10 years ago, and the drug has become a blockbuster for them, generating about a tenth of their entire revenue. The company has been promoting paroxetine directly to consumers as 'non-habit forming' for far too long."[10] Paroxetine prescribing information posted at GlaxoSmithKline now acknowledges the occurrence of a discontinuation syndrome, including serious discontinuation symptoms.[74]
Since the FDA approved paroxetine in 1992, approximately 5,000 U.S. citizens have sued GSK. Most of these people feel they were not sufficiently warned in advance of the drug's side effects—particularly the withdrawal syndrome discussed above, after GSK had specifically advertised the drug as non-habit forming.[69]
In 2001, GSK increased its American TV advertising of Paxil after the September 11 attacks; in October 2001, GSK spent nearly twice as much as in October 2000.[75] The difficulty of withdrawal from paroxetine, and GSK's concealment of it, was later reported on ABC.[76]
In the UK, since 2001 lawsuits have been filed representing people who have been prescribed Seroxat. They allege that the drug has serious side effects, which GlaxoSmithKline downplayed in patient information.[77][78]
In early 2004, GSK agreed to settle charges of consumer fraud for $2.5 million (a tiny fraction of the over $2.7 billion in yearly Paxil sales at that time).[79] The legal discovery process also uncovered evidence of deliberate, systematic suppression of unfavorable Paxil research results. One of GSK's internal documents had said, "It would be commercially unacceptable to include a statement that efficacy [in children] had not been demonstrated, as this would undermine the profile of paroxetine"[80].
In June 2004, FDA published a violation letter to GSK in response to a "false or misleading" TV ad for Paxil CR; FDA stated, "This ad is concerning from a public health perspective because it broadens the use of Paxil CR [beyond the conditions it was approved for] while also minimizing the serious risks associated with the drug."[81] GSK claimed the ad had been previously reviewed by FDA, but said the ad would not run again.[82]
On January 29, 2007, the BBC broadcast a fourth documentary in its Panorama series about the drug Seroxat.[83] This programme, entitled "Secrets of the Drug Trials", focused on three GSK paediatric clinical trials on depressed children and adolescents. Data from the trials show that Seroxat could not be proven to work for teenagers. Also, one clinical trial indicated that adolescents were six times more likely to become suicidal after taking it. Results from Study 329, one of the trials, were reported [84] in a way which misled readers about paroxetine's safety and efficacy, and contributed to repeated distortions in the assessment of the drug's value in paediatric depression in the scientific literature.[85]
The court documents released as a result of one of the lawsuits in October 2008 indicated that GSK "and/or researchers may have suppressed or obscured suicide risk data during clinical trials" of paroxetine. One of the investigators, "Charles Nemeroff, former chairman of the Department of Psychiatry at Emory University, was the first big name 'outed' ...In early October 2008, Nemeroff stepped down as department chair amid revelations that he had received over $960,000 from GSK in 2006, yet reported less than $35,000 to the school. Subsequent investigations revealed payments totaling more than $2.5 million from drug companies between 2000 and 2006, yet only a fraction was disclosed."[86]
The suppression of unfavorable research findings on Paxil by GSK — and the legal discovery process that uncovered it — is the subject of Alison Bass's 2008 book Side Effects: A Prosecutor, a Whistleblower, and a Bestselling Antidepressant on Trial[87].
Sales
In 2007, paroxetine was ranked 94th on the list of bestselling drugs, with over $1 billion in sales. In 2006, paroxetine was the fifth-most prescribed antidepressant in the United States retail market, with more than 19.7 million prescriptions.[88] In 2007, sales had dropped slightly to 18.1 million but paroxetine remained the fifth-most prescribed antidepressant in the U.S.[89]
Footnotes
- ↑ 1.0 1.1 Katzman MA (2009). "Current considerations in the treatment of generalized anxiety disorder". CNS Drugs 23 (2): 103–20. doi:10.2165/00023210-200923020-00002. PMID 19173371.
- ↑ Anderson IM (April 2000). "Selective serotonin reuptake inhibitors versus tricyclic antidepressants: a meta-analysis of efficacy and tolerability". J Affect Disord 58 (1): 19–36. doi:10.1016/S0165-0327(99)00092-0. PMID 10760555. http://linkinghub.elsevier.com/retrieve/pii/S0165-0327(99)00092-0.
- ↑ http://cat.inist.fr/?aModele=afficheN&cpsidt=972015
- ↑ Papakostas GI (2008). "Tolerability of modern antidepressants". J Clin Psychiatry 69 Suppl E1: 8–13. PMID 18494538.
- ↑ Barbui C, Furukawa TA, Cipriani A (January 2008). "Effectiveness of paroxetine in the treatment of acute major depression in adults: a systematic re-examination of published and unpublished data from randomized trials". CMAJ 178 (3): 296–305. doi:10.1503/cmaj.070693. PMID 18227449.
- ↑ 6.0 6.1 Hammad TA (2004-08-16). "Review and evaluation of clinical data: relationship between psychotropic drugs and pediatric suicidality" (PDF). Joint Meeting of the Psychopharmacologic Drugs Advisory Committee and Pediatric Advisory Committee. September 13–14, 2004. Briefing Information.. FDA. p. 30. http://www.fda.gov/ohrms/dockets/ac/04/briefing/2004-4065b1-10-TAB08-Hammads-Review.pdf. Retrieved 2009-01-27.
- ↑ Hammad TA, Laughren T, Racoosin J (March 2006). "Suicidality in pediatric patients treated with antidepressant drugs". Arch. Gen. Psychiatry 63 (3): 332–9. doi:10.1001/archpsyc.63.3.332. PMID 16520440.
- ↑ "Report of the CSM expert working group on the safety of selective serotonin reuptake inhibitor antidepressants" (PDF). MHRA. 2004-12. http://www.mhra.gov.uk/home/groups/pl-p/documents/drugsafetymessage/con019472.pdf. Retrieved 2009-02-17.
- ↑ 9.0 9.1 Haddad P (2001). "Antidepressant discontinuation syndromes". Drug Saf 24 (3): 183–97. doi:10.2165/00002018-200124030-00003. PMID 11347722.
- ↑ 10.0 10.1 10.2 10.3 Tonks A (February 2002). "Withdrawal from paroxetine can be severe, warns FDA". BMJ 324 (7332): 260. doi:10.1136/bmj.324.7332.260. PMID 11823353. PMC 1122195. http://bmj.com/cgi/pmidlookup?view=long&pmid=11823353.
- ↑ 11.0 11.1 ACOG Committee on Obstetric Practice (December 2006). "ACOG Committee Opinion No. 354: Treatment with selective serotonin reuptake inhibitors during pregnancy". Obstet Gynecol 108 (6): 1601–3. PMID 17138801.
- ↑ "FDA Public Health Advisory Paroxetine". Food and Drug Administration. http://www.fda.gov/Drugs/DrugSafety/PublicHealthAdvisories/ucm051731.htm. Retrieved 05/02/2009.
- ↑ "Paroxetine and Pregnancy". GlaxoSmithKline. http://www.gsk.com/media/paroxetine_pregnancy.htm. Retrieved 05/02/2009.
- ↑ Baldwin DS, Anderson IM, Nutt DJ, Bandelow B, Bond A, Davidson JR, den Boer JA, Fineberg NA, Knapp M, Scott J, Wittchen HU (2005). "Evidence-based guidelines for the pharmacological treatment of anxiety disorders: recommendations from the British Association for Psychopharmacology". Journal of Psychopharmacology 19 (6): 567–596. doi:10.1177/0269881105059253. PMID 16272179.
- ↑ D Baldwin, J Bobes, DJ Stein, I Scharwachter and M Faure (1999). "Paroxetine in social phobia/social anxiety disorder. Randomised, double-blind, placebo-controlled study. Paroxetine Study Group". The British Journal of Psychiatry 175: 120–126. doi:10.1192/bjp.175.2.120. PMID 10627793.
- ↑ Yonkers KA, Gullion C, Williams A, Novak K, Rush AJ. (1996). "Paroxetine as a treatment for premenstrual dysphoric disorder". Journal of Clinical Psychopharmacology. 16 (1): 3–8. doi:10.1097/00004714-199602000-00002. PMID 8834412.
- ↑ Turner, Francis Joseph (2005). Social Work Diagnosis in Contemporary Practice. Oxford University Press US. ISBN 019516878X.
- ↑ 18.0 18.1 18.2 18.3 18.4 18.5 "PAXIL (paroxetine hydrochloride) Tablets and Oral Suspension: PRESCRIBING INFORMATION" (PDF). Research Triangle Park, NC: GlaxoSmithKline. August 2007. http://us.gsk.com/products/assets/us_paxil.pdf. Retrieved 2007-08-14.
- ↑ Rapaport MH, Schneider LS, Dunner DL, Davies JT, Pitts CD (September 2003). "Efficacy of controlled-release paroxetine in the treatment of late-life depression". The Journal of Clinical Psychiatry 64 (9): 1065–74. doi:10.4088/JCP.v64n0912. PMID 14628982. http://www.psychiatrist.com/privatepdf/2003/v64n09/v64n0912.pdf.
- ↑ Waldinger MD, Hengeveld MW, Zwinderman AH, Olivier B (August 1998). "Effect of SSRI antidepressants on ejaculation: a double-blind, randomized, placebo-controlled study with fluoxetine, fluvoxamine, paroxetine, and sertraline". Journal of Clinical Psychopharmacology 18 (4): 274–81. doi:10.1097/00004714-199808000-00004. PMID 9690692.
- ↑ Waldinger MD, Zwinderman AH, Olivier B (2001). "SSRIs and ejaculation: a double-blind, randomized, fixed-dose study with paroxetine and citalopram". Journal of clinical psychopharmacology 21 (6): 556–60. doi:10.1097/00004714-200112000-00003. PMID 11763001.
- ↑ 22.0 22.1 Waldinger MD, Zwinderman AH, Olivier B (2004). "On-demand treatment of premature ejaculation with clomipramine and paroxetine: a randomized, double-blind fixed-dose study with stopwatch assessment". Eur. Urol. 46 (4): 510–5; discussion 516. doi:10.1016/j.eururo.2004.05.005. PMID 15363569.
- ↑ Brown J, O' Brien PM, Marjoribanks J, Wyatt K (2009). "Selective serotonin reuptake inhibitors for premenstrual syndrome". Cochrane Database Syst Rev (2): CD001396. doi:10.1002/14651858.CD001396.pub2. PMID 19370564.
- ↑ Kim SW, Grant JE, Adson DE, Shin YC, Zaninelli R (2002). "A double-blind placebo-controlled study of the efficacy and safety of paroxetine in the treatment of pathological gambling". Journal of Clinical Psychiatry 63 (6): 501–507. PMID 12088161.
- ↑ Weitzner MA, Moncello J, Jacobsen PB, Minton S. (2002). "A pilot trial of paroxetine for the treatment of hot flashes and associated symptoms in women with breast cancer". Journal of Pain and Symptom Management 23 (4): 337–345. doi:10.1016/S0885-3924(02)00379-2. PMID 11997203.
- ↑ Vieta E, Martinez-Aran A, Goikolea JM, Torrent C, Colom F, Benabarre A, Reinares M (1999). "The selective serotonin reuptake inhibitor paroxetine is effective in the treatment of diabetic neuropathy symptoms". Pain 42 (2): 135–144. doi:10.1016/0304-3959(90)91157-E. PMID 2147235.
- ↑ Langemark M, Olesen J (1994). "Sulpiride and paroxetine in the treatment of chronic tension-type headache. An explanatory double-blind trial". Headache 34 (1): 20–4. doi:10.1111/j.1526-4610.1994.hed3401020.x. PMID 8132436.
- ↑ Gartlehner G, Gaynes BN, Hansen RA, et al. (November 2008). "Comparative benefits and harms of second-generation antidepressants: background paper for the American College of Physicians". Ann. Intern. Med. 149 (10): 734–50. PMID 19017592. http://www.annals.org/cgi/content/full/149/10/734.
- ↑ http://www.nimh.nih.gov/health/topics/child-and-adolescent-mental-health/antidepressant-medications-for-children-and-adolescents-information-for-parents-and-caregivers.shtml
- ↑ http://www.pharmacytimes.com/issues/articles/2008-05_002.asp
- ↑ Masand PS, Gupta S (1999). "Selective serotonin-reuptake inhibitors: an update". Harv Rev Psychiatry 7 (2): 69–84. doi:10.1093/hrp/7.2.69. PMID 10471245.
- ↑ "Press release, CHMP meeting on Paroxetine and other SSRIs" (PDF). European Medicines Agency. 2004-12-09. http://www.emea.europa.eu/pdfs/human/press/pr/19257004en.pdf. Retrieved 2007-08-24.
- ↑ http://www.ncbi.nlm.nih.gov/books/bookres.fcgi/antidep/pdfantidep.pdf
- ↑ Olivera AA (May 1996). "A case of paroxetine-induced akathisia". Biol. Psychiatry 39 (10): 910. doi:10.1016/0006-3223(96)84504-5. PMID 8860197. http://linkinghub.elsevier.com/retrieve/pii/0006-3223(96)84504-5.
- ↑ Baldassano CF, Truman CJ, Nierenberg A, Ghaemi SN, Sachs GS (1996). "Akathisia: a review and case report following paroxetine treatment". Compr Psychiatry 37 (2): 122–4. doi:10.1016/S0010-440X(96)90572-6. PMID 8654061. http://linkinghub.elsevier.com/retrieve/pii/S0010-440X(96)90572-6.
- ↑ "Important Safety Information about Paxil CR". GlaxoSmithKline. http://www.paxilcr.com/safety_information/important_safety_information.html.
- ↑ Nishida T, Wada M, Wada M, Ito H, Narabayashi M, Onishi H (June 2008). "Activation syndrome caused by paroxetine in a cancer patient". Palliat Support Care 6 (2): 183–5. doi:10.1017/S1478951508000278. PMID 18501054. http://journals.cambridge.org/abstract_S1478951508000278.
- ↑ Ochiai Y, Katsu H, Okino S, Wakutsu N, Nakayama K (2003). "[Case of prolonged recovery from serotonin syndrome caused by paroxetine]" (in Japanese). Seishin Shinkeigaku Zasshi 105 (12): 1532–8. PMID 15027311.
- ↑ Terao T, Hikichi T (January 2007). "Serotonin syndrome in a case of depression with various somatic symptoms: the difficulty in differential diagnosis". Prog. Neuropsychopharmacol. Biol. Psychiatry 31 (1): 295–6. doi:10.1016/j.pnpbp.2006.07.007. PMID 16916568. http://linkinghub.elsevier.com/retrieve/pii/S0278-5846(06)00295-8.
- ↑ Clayton, A; Keller A, McGarvey EL. (2006). "Burden of phase-specific sexual dysfunction with SSRIs". Journal of Affective Disorders 91 (1): 27–32. doi:10.1016/j.jad.2005.12.007. PMID 16430968.
- ↑ http://findarticles.com/p/articles/mi_hb4365/is_1_42/ai_n31340240
- ↑ Vesely C, Fischer P, Goessler R, Kasper S (February 1997). "Mania associated with serotonin selective reuptake inhibitors". J Clin Psychiatry 58 (2): 88. PMID 9062382.
- ↑ Ramasubbu R (November 2004). "Antidepressant treatment-associated behavioural expression of hypomania: a case series". Prog. Neuropsychopharmacol. Biol. Psychiatry 28 (7): 1201–7. doi:10.1016/j.pnpbp.2004.06.015. PMID 15610935. http://linkinghub.elsevier.com/retrieve/pii/S0278-5846(04)00141-1.
- ↑ Grubbs JH (April 1997). "SSRI-induced mania". J Am Acad Child Adolesc Psychiatry 36 (4): 445. doi:10.1097/00004583-199704000-00003. PMID 9100415.
- ↑ Morishita S, Arita S (October 2003). "Induction of mania in depression by paroxetine". Hum Psychopharmacol 18 (7): 565–8. doi:10.1002/hup.531. PMID 14533140.
- ↑ Schmitt JA, Kruizinga MJ, Riedel WJ (September 2001). "Non-serotonergic pharmacological profiles and associated cognitive effects of serotonin reuptake inhibitors". J. Psychopharmacol. (Oxford) 15 (3): 173–9. doi:10.1177/026988110101500304. PMID 11565624.
- ↑ 47.0 47.1 "Anti-depressant addiction warning". BBC News. 2001-06-11. http://news.bbc.co.uk/1/hi/health/1382551.stm. Retrieved 2010-05-21.
- ↑ Skaehill, Penny A.; Welch, E.B. (October 1997). "Clinical Reviews: SSRI Withdrawal Syndrome". American Society of Consultant Pharmacists. http://www.ascp.com/publications/tcp/1997/oct/ssri.html. Retrieved 2007-08-15.
- ↑ Bhanji NH, Chouinard G, Kolivakis T, Margolese HC (2006). "Persistent tardive rebound panic disorder, rebound anxiety and insomnia following paroxetine withdrawal: a review of rebound-withdrawal phenomena". Can J Clin Pharmacol 13 (1): e69–74. PMID 16456219. http://www.cjcp.ca/pdf/CJCP_04-032_e69.pdf.
- ↑ http://apt.rcpsych.org/cgi/content/full/13/6/447
- ↑ http://www.benzo.org.uk/healy.htm
- ↑ http://www.medscape.com/viewarticle/498763
- ↑ 53.0 53.1 Thormahlen GM (October 2006). "Paroxetine use during pregnancy: is it safe?". Ann Pharmacother 40 (10): 1834–7. doi:10.1345/aph.1H116. PMID 16926304.
- ↑ Way CM (April 2007). "Safety of newer antidepressants in pregnancy". Pharmacotherapy 27 (4): 546–52. doi:10.1592/phco.27.4.546. PMID 17381382.
- ↑ 55.0 55.1 Bellantuono C, Migliarese G, Gentile S (April 2007). "Serotonin reuptake inhibitors in pregnancy and the risk of major malformations: a systematic review". Hum Psychopharmacol 22 (3): 121–8. doi:10.1002/hup.836. PMID 17397101.
- ↑ 56.0 56.1 Källén B (July 2007). "The safety of antidepressant drugs during pregnancy". Expert Opin Drug Saf 6 (4): 357–70. doi:10.1517/14740338.6.4.357. PMID 17688379.
- ↑ Bar-Oz B, Einarson T, Einarson A, et al (May 2007). "Paroxetine and congenital malformations: meta-Analysis and consideration of potential confounding factors". Clin Ther 29 (5): 918–26. doi:10.1016/j.clinthera.2007.05.003. PMID 17697910.
- ↑ Gentile S, Bellantuono C (March 2009). "Selective serotonin reuptake inhibitor exposure during early pregnancy and the risk of fetal major malformations: focus on paroxetine". J Clin Psychiatry 70 (3): 414–22. doi:10.4088/JCP.08r04468. PMID 19254517.
- ↑ PMID 19863482 (PubMed)
Citation will be completed automatically in a few minutes. Jump the queue or expand by hand - ↑ PMID 20513781 (PubMed)
Citation will be completed automatically in a few minutes. Jump the queue or expand by hand - ↑ 61.0 61.1 Einarson A, Selby P, Koren G (January 2001). "Abrupt discontinuation of psychotropic drugs during pregnancy: fear of teratogenic risk and impact of counselling". J Psychiatry Neurosci 26 (1): 44–8. PMID 11212593. PMC 1408034. http://www.cma.ca/multimedia/staticContent/HTML/N0/l2/jpn/vol-26/issue-1/pdf/pg44.pdf.
- ↑ Haddad PM, Pal BR, Clarke P, Wieck A, Sridhiran S (September 2005). "Neonatal symptoms following maternal paroxetine treatment: serotonin toxicity or paroxetine discontinuation syndrome?". J. Psychopharmacol. (Oxford) 19 (5): 554–7. doi:10.1177/0269881105056554. PMID 16166193.
- ↑ http://us.gsk.com/products/assets/us_paxil.pdf
- ↑ BMJ 2010;340:c693
- ↑ Mellerup, Erling T.; Plenge, Per (July 1986). "High affinity binding of3H-paroxetine and3H-imipramine to rat neuronal membranes". Psychopharmacology (Springer Berlin / Heidelberg) 89 (4): 436–439. doi:10.1007/BF02412117. PMID 2944152. http://www.springerlink.com/content/5888x32v705t336r/.
- ↑ Golden RN, Nemeroff CB, McSorley P, Pitts CD, Dube EM. (2002). "Efficacy and tolerability of controlled-release and immediate-release paroxetine in the treatment of depression". Journal of Clinical Psychiatry 63 (7): 577–584. PMID 12143913.
- ↑ Goeringer KE, Raymon L, Christian GD, Logan BK. Postmortem forensic toxicology of selective serotonin reuptake inhibitors: a review of pharmacology and report of 168 cases. J. For. Sci. 45: 633-648, 2000.
- ↑ R. Baselt, Disposition of Toxic Drugs and Chemicals in Man, 8th edition, Biomedical Publications, Foster City, CA, 2008, pp. 1190-1193.
- ↑ 69.0 69.1 "Judge: Paxil ads can't say it isn't habit-forming". USA Today. 2002-08-20. http://www.usatoday.com/news/health/2002-08-20-paxil-ads_x.htm. Retrieved 2010-05-21.
- ↑ http://www.socialaudit.org.uk/4606-BAUM%20HEDLUND.htm
- ↑ http://www.citypages.com/2002-10-16/news/paxil-is-forever/
- ↑ "Anti-depressant addiction warning". BBC News. 2001-06-11. http://news.bbc.co.uk/2/hi/health/1382551.stm. Retrieved 2010-03-27.
- ↑ http://findarticles.com/p/articles/mi_qa4070/is_200206/ai_n9121579
- ↑ Paxil (paroxetine hydrochloride) prescribing information
- ↑ "Drug Makers Find Sept. 11 A Marketing Opportunity". Psychiatric News. 1 March 2001. http://pn.psychiatryonline.org/cgi/content/full/37/5/9. Retrieved 12 July 2010.
- ↑ http://www.youtube.com/watch?v=xSUAsdBgh70
- ↑ Garfield, Simon (2002-04-29). "The Chemistry of Happiness". London: The Guardian. http://society.guardian.co.uk/mentalhealth/story/0,,707016,00.html. Retrieved 2007-09-09.
- ↑ Stayton, Jonathan (2008-01-22). "Punk rocker sues over anti-depressant". The Argus. http://www.theargus.co.uk/news/generalnews/display.var.1984445.0.punk_rocker_sues_over_antidepressant.php. Retrieved 2008-01-23.
- ↑ Angell, Marcia (2009), "Drug Companies & Doctors: A Story of Corruption", New York Review of Books, Vol 56, No 1; 15 January 2009.
- ↑ Kondro W, Sibbald B (March 2004). "Drug company experts advised staff to withhold data about SSRI use in children". CMAJ 170 (5): 783. doi:10.1503/cmaj.1040213. PMID 14993169. PMC 343848. http://www.cmaj.ca/cgi/pmidlookup?view=long&pmid=14993169.
- ↑ http://www.fda.gov/downloads/Drugs/GuidanceComplianceRegulatoryInformation/EnforcementActivitiesbyFDA/WarningLettersandNoticeofViolationLetterstoPharmaceuticalCompanies/ucm055293.pdf
- ↑ "Company News; F.D.A. Asks Glaxosmithkline To Stop Running A Paxil Ad". The New York Times. 2004-06-12. http://www.nytimes.com/2004/06/12/business/company-news-fda-asks-glaxosmithkline-to-stop-running-a-paxil-ad.html. Retrieved 2010-03-27.
- ↑ "Secrets of the drug trials". BBC. 2007-01-29. http://news.bbc.co.uk/1/hi/programmes/panorama/6291773.stm. Retrieved 2007-08-15.
- ↑ Keller MB et al (July 2001). "Efficacy of paroxetine in the treatment of adolescent major depression: a randomized, controlled trial". J Am Acad Child Adolesc Psychiatry 40 (7): 762–72. doi:10.1097/00004583-200107000-00010. PMID 11437014.
- ↑ http://healthyskepticism.org/documents/PaxilStudy329.php
- ↑ Kurt Sammson (December 2008). "SENATE PROBE SEEKS INDUSTRY PAYMENT DATA ON INDIVIDUAL ACADEMIC RESEARCHERS". Annals of neurology: A7.
- ↑ Bass, Alison (2008), Side Effects: A Prosecutor, a Whistleblower, and a Bestselling Antidepressant on Trial, Algonquin Books of Chapel Hill.
- ↑ The paroxetine prescriptions were calculated as a total of prescriptions for Paxil CR and generic paroxetine using data from the charts for generic and brand-name drugs."Top 200 generic drugs by units in 2006. Top 200 brand-name drugs by units.". Drug Topics, Mar 5, 2007. http://www.drugtopics.com/drugtopics/article/articleDetail.jsp?id=407652. Retrieved 2007-04-08.
- ↑ The paroxetine prescriptions were calculated as a total of prescriptions for Paxil CR and generic paroxetine using data from the charts for generic and brand-name drugs."Top 200 generic drugs by units in 2007.". Drug Topics, Feb 18, 2008. http://drugtopics.modernmedicine.com/drugtopics/Top200Drugs/ArticleStandard/article/detail/491194. Retrieved 2008-10-23. "Top 200 brand drugs by units in 2007.". Drug Topics, Feb 18, 2008. http://drugtopics.modernmedicine.com/drugtopics/PharmacyFactsAndFigures/ArticleStandard/article/detail/491210. Retrieved 2008-10-23.
External links
- List of international brand names for paroxetine
- Detailed Paroxetine Consumer Information: Uses, Precautions, Side Effects from medlibrary.org
- The Secrets of Seroxat, BBC Panorama investigation
- Antidepressant Use in Children Soars Despite Efficacy Doubts, Washington Post, April 18, 2004
- Healthy Skepticism's repository and analysis of GSK documents related to Study 329
|
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|
|||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||